Introduction
Diabetes mellitus, commonly referred to as diabetes, is a chronic metabolic disorder that affects millions of people worldwide. It is characterized by elevated blood sugar levels due to the body’s inability to produce or due to resistance to insulin or both. In this comprehensive blog post, we will delve into the different types of diabetes, explore their causes, discuss the pathophysiology of the disease, highlight treatment options, and shed light on the potential complications associated with diabetes mellitus.
Types of Diabetes
Diabetes mellitus is classified into several types, including:
Type 1 Diabetes Mellitus / Insulin-Dependent Diabetes Mellitus (IDDM)
It is an autoimmune condition where the body’s immune system attacks and destroys insulin-producing cells in the pancreas. Individuals with IDDM rely on insulin injections or Insulin pumps to manage their blood sugar levels. This type typically manifests in childhood or early adulthood and requires lifelong insulin therapy.
Type 2 Diabetes Mellitus / Non-insulin-dependent diabetes
This type is the most common form, characterized by insulin resistance and inadequate insulin production. Lifestyle factors, such as obesity and sedentary behavior, play a significant role in its development. Type 2 diabetes can often be managed through dietary modifications, exercise, oral medications, and, in some cases, insulin therapy.
Gestational Diabetes Mellitus
Develops during pregnancy and usually resolves six weeks after childbirth. This condition should manage with medical nutrition therapy, metformin oral drug or insulin therapy, or a suitable combination under consultant supervision.
MODY / Maturity onset diabetes of young
In simple terms, this can explain as type 2 diabetes occurs at a young age. Present due to a sedentary lifestyle and obesity young people will commonly have type 2 diabetes mellitus.
LADA / Latent Autoimmune Diabetes of adults
In simple terms, it is same as the type 1 diabetes mellitus. But it occurs in later life. Type 1 occurs at young ages. That is the difference between type 1 and LADA. This is also an autoimmune condition.
Causes of Diabetes Mellitus
Diabetes mellitus is a complex condition influenced by various factors, including genetics, lifestyle choices, and environmental triggers. Understanding these causes can help individuals take proactive steps in preventing or managing the disease.
Genetic Factors
There is a strong genetic component in the development of diabetes mellitus. Certain genes and gene variations can increase an individual’s susceptibility to the disease. For instance, type 1 diabetes has a significant genetic predisposition, with specific human leukocyte antigen (HLA) genes playing a crucial role. In type 2 diabetes, multiple genes contribute to insulin resistance and impaired insulin secretion. However, having these genetic factors does not guarantee the development of diabetes; other triggers are often required.
Insulin Resistance
Insulin resistance is a key factor in the development of type 2 diabetes mellitus. It occurs when the body’s cells become less responsive to the action of insulin, resulting in elevated blood sugar levels. The exact causes of insulin resistance are not fully understood, but several factors contribute to its development. These include obesity, particularly excess abdominal fat, a sedentary lifestyle, unhealthy dietary habits (such as a high intake of processed foods, sugary beverages, and saturated fats), and chronic inflammation.
Beta Cell Dysfunction
In both type 1 and type 2 diabetes mellitus, dysfunction or destruction of the insulin-producing beta cells in the pancreas can contribute to the disease. In type 1 diabetes, the immune system mistakenly attacks and destroys these cells, resulting in a complete lack of insulin production. The exact triggers for this autoimmune response are not well defined, but genetic susceptibility, viral infections, and environmental factors may play a role. In type 2 diabetes, the beta cells may initially produce sufficient insulin, but over time, they become exhausted and produce less insulin or release it less efficiently.
Obesity and Body Fat Distribution
Obesity is a significant risk factor for developing type 2 diabetes mellitus. Excess body fat, particularly visceral fat (fat around the abdominal organs), contributes to insulin resistance and metabolic dysfunction. Adipose tissue releases various hormones and chemicals that interfere with insulin signaling and glucose metabolism. Additionally, obesity is associated with chronic low-grade inflammation, further impairing insulin action. Maintaining a healthy weight through regular physical activity and a balanced diet is crucial in reducing the risk of developing type 2 diabetes.
Environmental Factors
Certain environmental factors can contribute to the development of diabetes mellitus. These include exposure to certain viruses and toxins, such as enteroviruses and chemicals found in some pesticides. Viral infections may trigger an autoimmune response, leading to the destruction of beta cells in susceptible individuals. Environmental pollutants, such as persistent organic pollutants (POPs) and heavy metals, have also been implicated in insulin resistance and diabetes development.
It’s important to note that while these factors contribute to the development of diabetes mellitus, they may interact differently in each individual. Some people may have a genetic predisposition but never develop diabetes, while others may develop the disease despite having few known risk factors. Taking a holistic approach to diabetes prevention and management, including maintaining a healthy lifestyle and regular medical check-ups, is crucial for reducing the risk and effectively managing diabetes mellitus.
Pathophysiology of Diabetes Mellitus
The pathophysiology of diabetes mellitus involves a complex interplay of various factors that lead to impaired insulin action, inadequate insulin secretion, and abnormal glucose metabolism. Understanding the underlying mechanisms can provide insights into the disease progression and guide treatment strategies.
Insulin Resistance
Insulin resistance is a key characteristic of type 2 diabetes mellitus and occurs when the body’s cells become less responsive to the action of insulin. It primarily affects muscle, liver, and adipose tissue. Multiple factors contribute to insulin resistance, including obesity, chronic inflammation, genetic predisposition, and hormonal imbalances.
In obesity, excess adipose tissue releases inflammatory cytokines and free fatty acids. These substances interfere with insulin signaling pathways, leading to impaired glucose uptake in muscle cells and increased glucose production by the liver. Insulin resistance in adipose tissue further contributes to the increased release of fatty acids, exacerbating the problem.
Beta Cell Dysfunction
Beta cells in the pancreas play a crucial role in producing and releasing insulin. In both type 1 and type 2 diabetes, beta cell dysfunction contributes to the pathophysiology of the disease.
In type 1 diabetes, an autoimmune process leads to the destruction of beta cells. The immune system mistakenly identifies these cells as foreign and launches an attack, resulting in a complete lack of insulin production. This autoimmune response is thought to be triggered by genetic susceptibility and environmental factors, such as viral infections.
In type 2 diabetes, beta cell dysfunction occurs due to a combination of factors. Initially, the beta cells may produce excessive amounts of insulin to compensate for insulin resistance. However, over time, they become exhausted and are unable to secrete adequate amounts of insulin. Additionally, chronic hyperglycemia (high blood sugar) can impair beta cell function and promote cell death.
Glucose Overproduction
In diabetes mellitus, there is often an overproduction of glucose by the liver, contributing to elevated blood sugar levels. In individuals with insulin resistance, the liver fails to respond to the suppressive effect of insulin on glucose production. As a result, the liver continues to release glucose into the bloodstream, even when blood sugar levels are already high.
Glucose Uptake and Utilization
Impaired glucose uptake by muscle cells is a hallmark of insulin resistance. Normally, insulin facilitates the entry of glucose into muscle cells, where it is used as a source of energy. However, in insulin-resistant individuals, this process is disrupted, and glucose uptake is reduced. As a result, glucose remains elevated in the bloodstream, leading to hyperglycemia.
Abnormal Glucagon Secretion
Glucagon, a hormone produced by the alpha cells of the pancreas, has the opposite effect of insulin. It raises blood sugar levels by promoting the breakdown of glycogen stored in the liver, releasing glucose into the bloodstream. In diabetes, there can be abnormal glucagon secretion, contributing to increased glucose production and further elevating blood sugar levels.
Impaired Incretin Hormone Function
Incretin hormones, such as glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP), play a vital role in regulating glucose metabolism. They stimulate insulin release from beta cells, suppress glucagon secretion, slow down gastric emptying, and promote satiety. In type 2 diabetes, there is often impaired incretin hormone function, leading to reduced insulin secretion and diminished glucose regulation.
Understanding the pathophysiology of diabetes mellitus helps healthcare professionals develop targeted treatment strategies. By addressing insulin resistance, enhancing beta cell function, and managing glucose production and utilization, it is possible to improve blood sugar control and mitigate the complication
Diabetes Mellitus Symptoms
Recognizing the signs and symptoms of diabetes mellitus is crucial for early diagnosis and prompt treatment. Common symptoms include excessive thirst, frequent urination, unexplained weight loss, fatigue, blurred vision, slow wound healing, and recurrent infections. However, some individuals with type 2 diabetes may exhibit no symptoms initially, making regular screenings important.
Treatment Options for Diabetes Mellitus
Diabetes mellitus treatment aims to maintain blood sugar levels within a target range to prevent complications. The treatment plan may include:
Medications
Oral antidiabetic drugs, injectable medications, and insulin therapy are prescribed based on the type and severity of diabetes.
Lifestyle Modifications
A balanced diet, regular exercise, weight management, and stress reduction are crucial components of diabetes management.
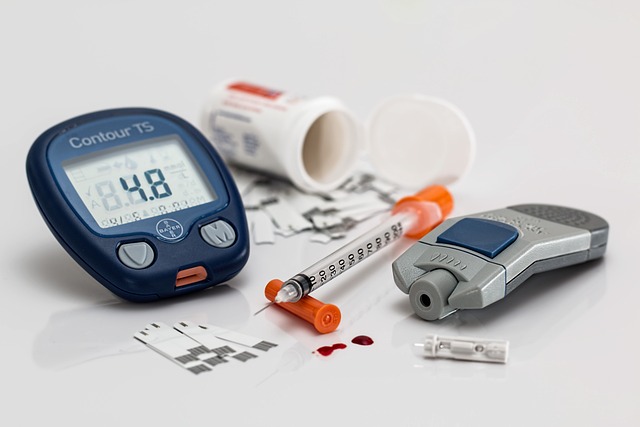
Blood Sugar Monitoring
Regular monitoring helps individuals track their blood glucose levels and make necessary adjustments to their treatment plans.
Complications of Diabetes Mellitus
Uncontrolled diabetes can lead to various complications that affect multiple organ systems. These complications include macrovascular and microvascular complications both.
Macrovascular complications
- Cardiovascular Complications: Increased risk of heart disease, stroke, and peripheral arterial disease.
Microvascular complications
- Diabetic Retinopathy: Damage to the blood vessels in the retina, leading to vision impairment and blindness.
- Diabetic Neuropathy: Nerve damage resulting in tingling, numbness, pain, or loss of sensation in the extremities.
- Diabetic Nephropathy: Kidney damage that can progress to chronic kidney disease or end-stage renal disease.
Commonly Asked Questions by patients during clinic visits and health education sessions.
What is diabetes?
Diabetes is a chronic metabolic disorder characterized by elevated blood sugar levels. It occurs when the body either doesn’t produce enough insulin (a hormone that regulates blood sugar) or doesn’t effectively use the insulin it produces.
What are the different types of diabetes?
The main types of diabetes are:
- Type 1 Diabetes: An autoimmune condition where the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas.
- Type 2 Diabetes: The most common form, characterized by insulin resistance and inadequate insulin production.
- Gestational Diabetes: Develops during pregnancy and usually resolves after childbirth.
- Other Types
What are the symptoms of diabetes?
Common symptoms of diabetes include frequent urination, excessive thirst, unexplained weight loss, increased hunger, fatigue, blurry vision, slow wound healing, and frequent infections.
How is diabetes diagnosed?
Diabetes can be diagnosed through various tests, including fasting blood sugar test, oral glucose tolerance test, and hemoglobin A1c test. These tests measure blood sugar levels and help determine if someone has diabetes.
What causes diabetes?
The causes of diabetes vary depending on the type. Type 1 diabetes is believed to result from a combination of genetic predisposition and environmental triggers. Type 2 diabetes is influenced by genetic factors, obesity, a sedentary lifestyle, poor dietary habits, and other environmental factors.
Can diabetes be prevented?
While type 1 diabetes cannot be prevented, type 2 diabetes can often be prevented or delayed through lifestyle modifications such as maintaining a healthy weight, engaging in regular physical activity, and following a balanced diet.
What are the risk factors for developing diabetes?
Risk factors for diabetes include a family history of diabetes, obesity, a sedentary lifestyle, unhealthy eating habits, high blood pressure, ethnicity (certain ethnic groups have higher risk), and a history of gestational diabetes.
What is the role of insulin in diabetes?
Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels. In diabetes, either the body doesn’t produce enough insulin (type 1) or the body becomes resistant to the effects of insulin (type 2). Insulin therapy is often used to manage diabetes.
How is diabetes treated?
Diabetes treatment depends on the type and severity of the condition. It may involve lifestyle modifications (healthy eating, regular exercise), oral medications (for type 2 diabetes), insulin therapy (for type 1 diabetes or advanced type 2 diabetes), blood sugar monitoring, and regular medical check-ups.
What lifestyle changes are recommended for managing diabetes?
Lifestyle changes for managing diabetes include adopting a healthy diet (rich in fruits, vegetables, whole grains, and lean proteins), engaging in regular physical activity, maintaining a healthy weight, managing stress, getting enough sleep, and avoiding tobacco and excessive alcohol consumption
What is the importance of diet and exercise in diabetes management?
Diet and exercise play crucial roles in diabetes management. A balanced diet helps regulate blood sugar levels and manage weight, while regular exercise improves insulin sensitivity and helps control blood sugar. It is important to work with a healthcare team to develop a personalized plan.
Can diabetes be cured?
Currently, there is no cure for diabetes. However, with proper management, lifestyle changes, and medical treatment, diabetes can be effectively controlled, and individuals can live healthy and fulfilling lives.
Are there any complications associated with diabetes?
Yes, diabetes can lead to various complications if not properly managed. These complications can affect the eyes (diabetic retinopathy), kidneys (diabetic nephropathy), nerves (diabetic neuropathy), and cardiovascular system (heart disease and stroke). It can also increase the risk of foot problems, skin conditions, and other health issues.
What are the long-term effects of poorly controlled diabetes?
Poorly controlled diabetes can lead to serious long-term complications. These include kidney damage, nerve damage, vision loss, heart disease, stroke, foot ulcers, and amputation. It is important to maintain good blood sugar control to reduce the risk of these complications.
How often should I check my blood sugar levels?
The frequency of blood sugar monitoring depends on the type of diabetes, treatment plan, and individual circumstances. It is typically recommended to check blood sugar levels regularly, such as before meals, after meals, and at bedtime. Your healthcare provider can provide specific guidance.
What should my target blood sugar range be?
Target blood sugar ranges vary depending on factors such as age, overall health, and diabetes management goals. Generally, fasting blood sugar levels should be between 80-130 mg/dL (4.4-7.2 mmol/L), and post-meal levels should be below 180 mg/dL (10 mmol/L). It’s important to discuss and set specific targets with your healthcare provider.
What are the potential side effects of diabetes medications?
Different diabetes medications may have different side effects. Common side effects include low blood sugar (hypoglycemia), gastrointestinal issues (such as nausea or diarrhea), weight gain, and skin reactions. It’s important to discuss potential side effects with your healthcare provider.
Is it safe to take insulin?
Yes, insulin is safe when prescribed and used appropriately. It is a vital treatment for individuals with type 1 diabetes and is often used in type 2 diabetes when other treatments are insufficient. Proper education and guidance from healthcare professionals are important for its safe and effective use.
Can I still lead a normal life with diabetes?
Yes, with proper management, people with diabetes can lead normal, active lives. It is essential to maintain good blood sugar control, follow a healthy lifestyle, and work closely with healthcare professionals to prevent complications and achieve optimal health.
How can I manage diabetes while traveling?
Managing diabetes while traveling requires planning and preparation. Carry necessary supplies, medication, and snacks. Have a travel plan, adjust medication schedules across time zones if needed, stay hydrated, and be aware of local healthcare resources. Consult your healthcare team for personalized advice.
Can I drink alcohol if I have diabetes?
Moderate alcohol consumption may be possible for some individuals with diabetes, but it requires caution. Alcohol can affect blood sugar levels, interact with medications, and contribute to weight gain. It is important to discuss alcohol consumption with your healthcare provider and monitor its effects on your blood sugar.
How does diabetes affect pregnancy?
Diabetes mellitus can have implications for pregnancy. Gestational diabetes can develop during pregnancy, and pre-existing diabetes (type 1 or type 2) can impact pregnancy outcomes. It requires careful management to ensure optimal maternal and fetal health. Pregnant women with diabetes should work closely with their healthcare team to monitor blood sugar levels and adjust treatment as needed.
Is it possible to have diabetes without experiencing symptoms?
Yes, it is possible to have diabetes mellitus without experiencing noticeable symptoms, particularly in the early stages. This is especially true for type 2 diabetes, which often develops gradually. Regular health check-ups and blood sugar screenings are important for early detection, especially for individuals with risk factors.
Are there any natural remedies or alternative treatments for diabetes?
While certain natural remedies and alternative treatments may complement conventional diabetes management, it is crucial to consult with a healthcare provider before trying any new approach. Some approaches, such as dietary modifications, regular exercise, stress management techniques, and certain supplements, may have potential benefits, but they should not replace medical advice or prescribed treatments.
Where can I find support and resources for living with diabetes?
There are numerous resources available to support individuals living with diabetes. These include diabetes education centers, support groups, online communities, reputable websites, and national diabetes associations. Your healthcare provider can provide recommendations and referrals to local resources that can help you navigate life with diabetes.
Summary
Diabetes mellitus is a chronic metabolic disorder characterized by elevated blood sugar levels, resulting from the body’s inability to produce or effectively use insulin. This comprehensive article explores the different types of diabetes, their causes, pathophysiology, treatment options, and potential complications.
The main types of diabetes discussed are Type 1, Type 2, gestational diabetes, MODY, and LADA. Genetic factors play a significant role in the development of diabetes, along with insulin resistance, beta cell dysfunction, obesity, and environmental factors such as viral infections and exposure to certain toxins.
The pathophysiology of diabetes involves insulin resistance, beta cell dysfunction, glucose overproduction, impaired glucose uptake and utilization, abnormal glucagon secretion, and impaired incretin hormone function. Understanding these mechanisms is crucial for designing targeted treatment strategies to control blood sugar levels effectively.
The treatment options for diabetes include medications (oral antidiabetic drugs, injectable medications, and insulin therapy), lifestyle modifications (diet, exercise, weight management, stress reduction), and regular blood sugar monitoring. Early diagnosis and prompt treatment are important to prevent complications.
Uncontrolled diabetes can lead to macrovascular and microvascular complications. Macrovascular complications include an increased risk of heart disease, stroke, and peripheral arterial disease. Microvascular complications involve diabetic retinopathy, diabetic neuropathy, and diabetic nephropathy, which affect the eyes, nerves, and kidneys, respectively.
The article also addresses commonly asked questions about diabetes, including its types, symptoms, diagnosis, prevention, risk factors, the role of insulin, treatment options, the importance of diet and exercise, potential complications, and the long-term effects of poorly controlled diabetes.
In conclusion, this comprehensive article provides valuable information about diabetes mellitus, including its types, causes, pathophysiology, treatment options, and potential complications. By understanding the disease and taking appropriate measures, individuals can effectively manage diabetes and reduce the risk of complications, leading to a healthier and more fulfilling life.

It’s difficult to find well-informed people for this topic,
however, you seem like you know what you’re talking about!
Thanks
I think this is one of the most important info for me.
And i’m glad reading your article. But wanna remark on some general
things, The website style is great, the articles is really excellent :
D. Good job, cheers
Hiya! Quick question that’s entirely off topic. Do you know how to make your site mobile friendly?
My blog looks weird when viewing from my apple
iphone. I’m trying to find a theme or plugin that might be able to resolve this issue.
If you have any suggestions, please share. Cheers!
You made some really good points there. I checked on the internet
to learn more about the issue and found most people will go along with your views on this
website.