We’ve all had a cut, scrape, or burn that seems to take forever to heal. While most minor injuries repair themselves within a couple of weeks, some wounds stubbornly refuse to close, lingering for months or even years. This frustrating condition is known as delayed wound healing or a chronic wound, and it’s more than just an inconvenience—it can be a significant warning sign from your body.
If you’re caring for a wound that isn’t progressing, you’re not alone. Understanding the “why” behind the delay is the first, most powerful step toward getting back on the path to healing.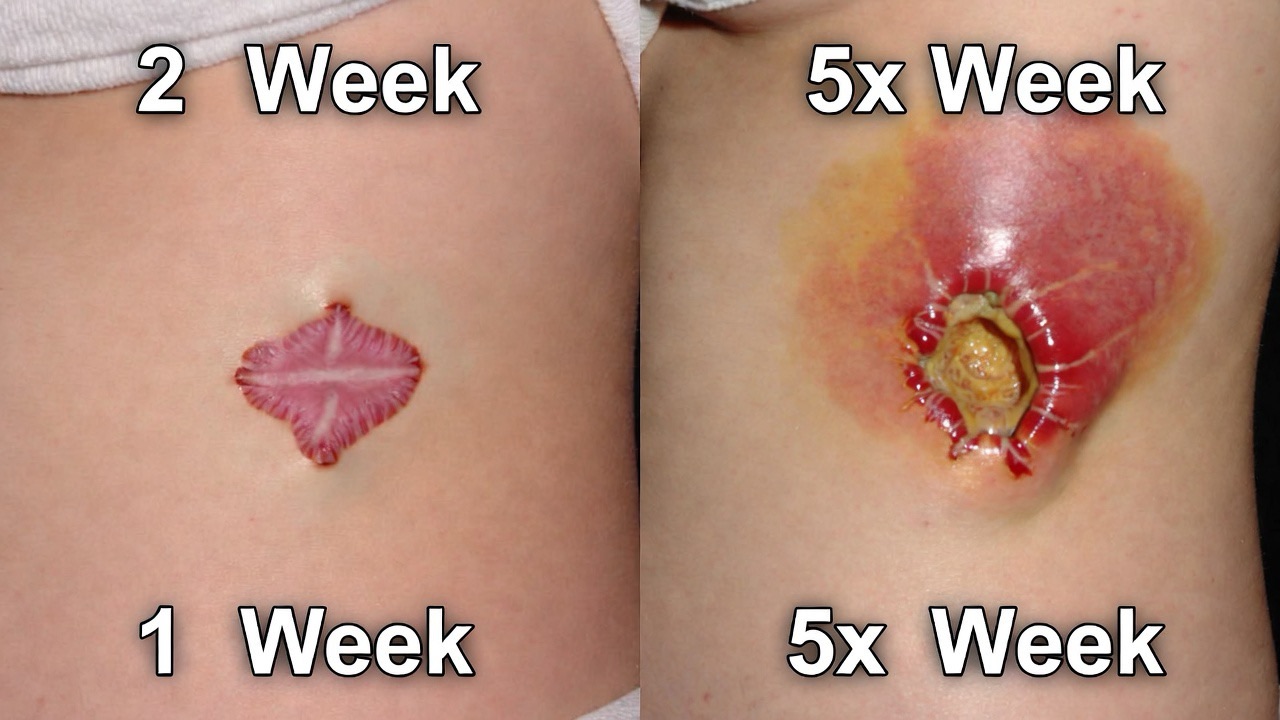
The Basics: How Is a Wound Supposed to Heal?
Normal wound healing is a beautiful, complex dance that happens in four predictable stages:
1. Hemostasis (Stop the Bleeding): Blood vessels constrict, and platelets form a clot.
2. Inflammation (Clean the Site): The area becomes red, warm, and slightly swollen as white blood cells arrive to fight infection.
3. Proliferation (Rebuild): New tissue (granulation tissue) fills the wound, and skin cells migrate from the edges to close it.
4. Maturation (Strengthen): The new tissue remodels and gains strength over months.
A chronic wound gets “stuck,” usually in the inflammatory or proliferative stage, unable to move forward.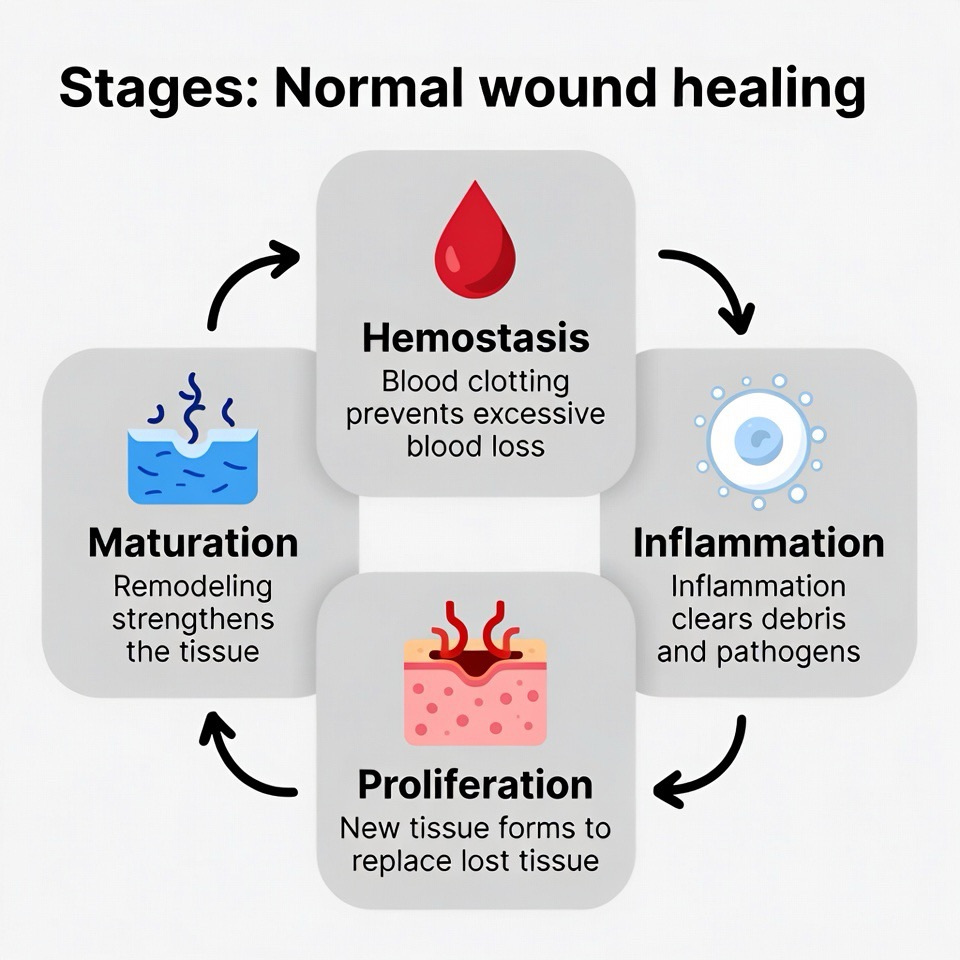
The Top 7 Causes of Delayed Wound Healing
1. Infection
This is the most common culprit. Bacteria in a wound create a constant state of inflammation, hijacking the body’s resources to fight invaders instead of building new tissue.
· Signs: Increased pain, redness, warmth, swelling, foul-smelling or colored discharge (yellow/green pus), and sometimes fever.
2. Poor Blood Circulation
Think of blood as the delivery service for oxygen and nutrients—the essential building blocks for healing. Conditions that impair circulation starve the wound.
· Related Conditions: Peripheral Artery Disease (PAD), diabetes, smoking, and atherosclerosis.
· Common Sites: Wounds on the lower legs and feet (often called venous stasis ulcers or arterial ulcers).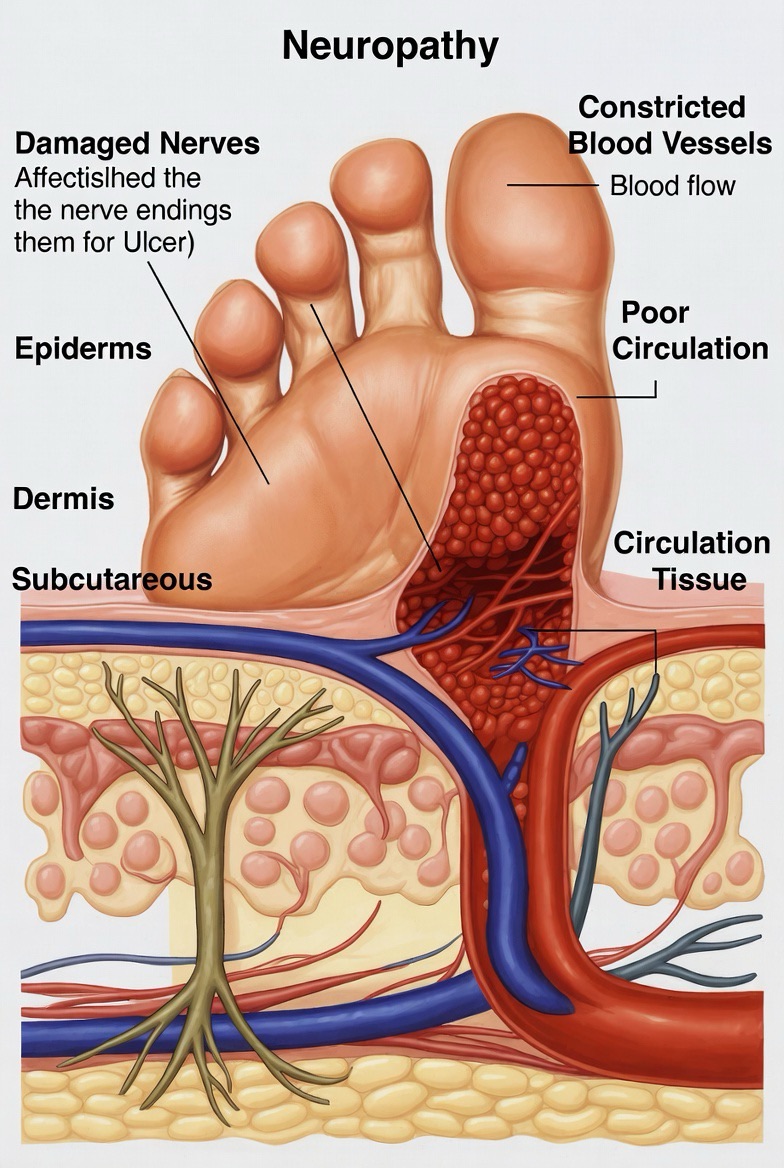
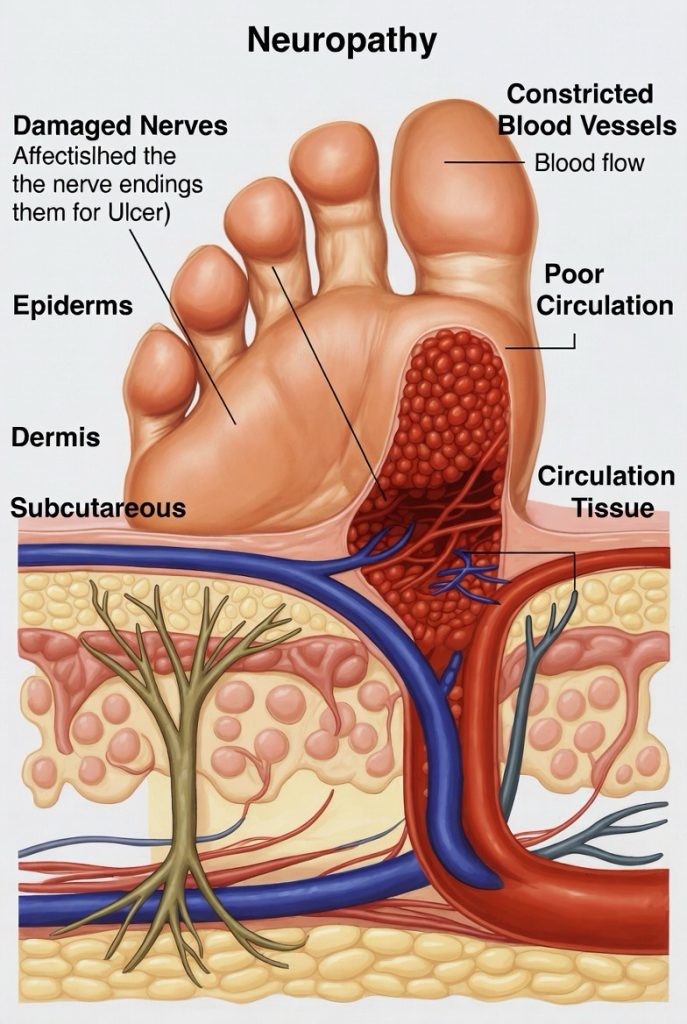
3. Diabetes
Diabetes is a triple threat to wound healing:
· Poor Circulation: High blood sugar damages blood vessels.
· Nerve Damage (Neuropathy): Reduces sensation, so injuries go unnoticed and worsen.
· Weakened Immune Response: Increases risk of severe infection.
A non-healing foot ulcer is a major complication of diabetes and requires immediate, specialized care.
4. Repeated Trauma or Pressure
If a wound is constantly being reopened, rubbed, or pressed upon, it can’t stabilize enough to heal.
· Example: A blister on the heel from a shoe that keeps rubbing, or a pressure ulcer (bed sore) in a bedridden patient from unrelieved pressure.
5. Nutritional Deficiencies
Your body needs specific nutrients to synthesize new cells and tissue.
· Key Players: Protein, Vitamin C, Zinc, and Vitamin A. Chronic malnutrition or restrictive diets can significantly slow repair.
6. Certain Medications
Some drugs, while necessary, can interfere with the healing cascade.
· Examples: Long-term use of corticosteroids (like prednisone), some chemotherapy drugs, and some anti-inflammatory medications.
7. Underlying Health Conditions
Systemic diseases can divert the body’s energy and resources away from healing.
· Examples: Autoimmune diseases (like lupus or rheumatoid arthritis), kidney failure, anemia, and cancer.
What to Do: A Step-by-Step Action Plan
If your wound hasn’t shown improvement in 2-4 weeks, it’s time to take deliberate action.
Step 1: Seek Professional Medical Evaluation
This is non-negotiable. Don’t try to diagnose or treat a chronic wound alone. Start with your primary care doctor. They may refer you to a:
· Wound Care Specialist (often at a dedicated Wound Care Center)
· Dermatologist (for skin-related issues)
· Vascular Surgeon (for circulation problems)
· Podiatrist (for foot wounds, especially related to diabetes)
Step 2: Optimize Your At-Home Wound Care (Under Guidance)
Your healthcare team will create a plan, which will likely include:
· Proper Cleaning: Gently cleaning with saline or a recommended cleanser daily.
· Moist Wound Healing: Using modern dressings (like hydrocolloids or foams) that maintain a moist environment, which has been proven to speed healing far more than letting a wound dry out and scab.
· Protection: Keeping the wound covered with a clean, appropriate dressing and protecting it from trauma.
· Never Using Harmful Agents: Avoid hydrogen peroxide or iodine on chronic wounds, as they can damage fragile new tissue cells.
Step 3: Address the Root Cause
Treating the wound without treating the cause is like bailing water from a leaking boat without plugging the hole. Your doctor will help you manage:
· Blood Sugar if you have diabetes.
· Circulation issues.
· Nutritional deficiencies with supplements or diet changes.
· Infection with targeted antibiotics.
Step 4: Support Your Body’s Healing Ability
· Eat a Healing Diet: Prioritize lean protein (chicken, fish, beans), colorful fruits and vegetables (for Vitamin C), and whole grains.
· Stop Smoking: Nicotine constricts blood vessels, drastically reducing blood flow to the skin.
· Manage Underlying Conditions: Strictly follow treatment plans for diabetes, heart disease, etc.
· Offload Pressure: For foot or leg wounds, you may need special footwear or devices to keep pressure off the area.
When Is It a Medical Emergency?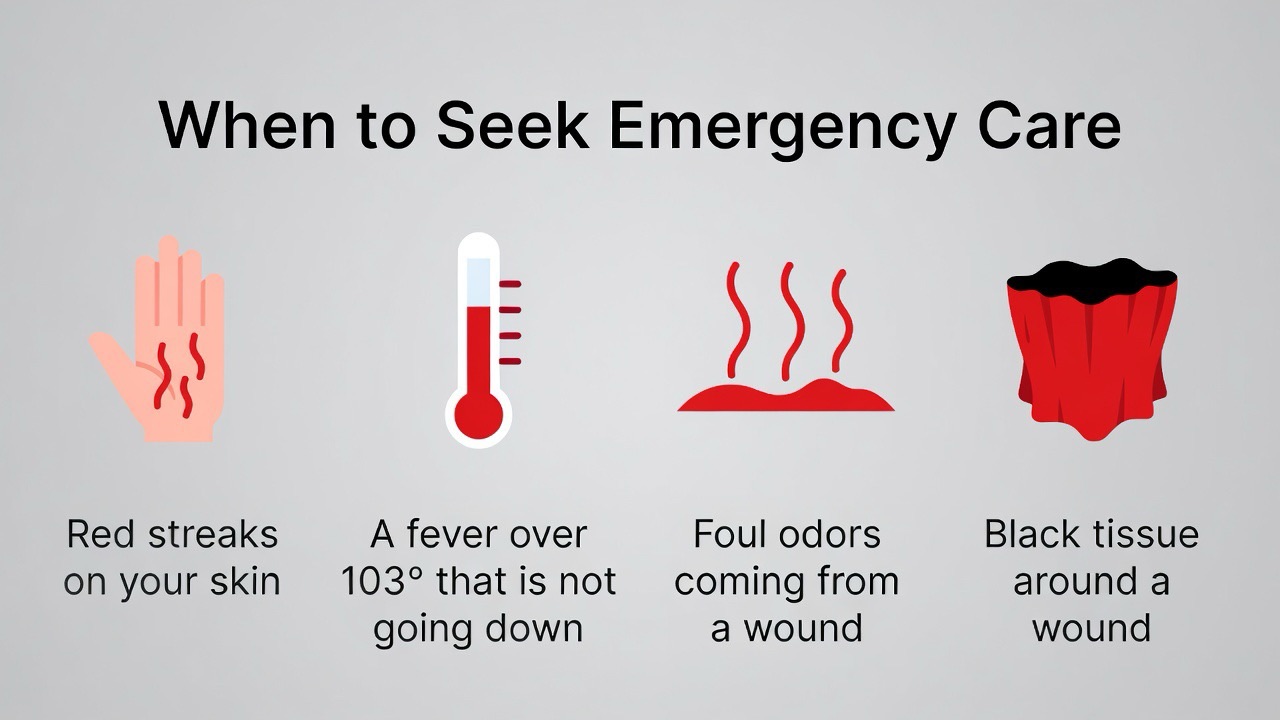
Go to the emergency room or seek immediate care if the wound shows signs of a deep or spreading infection:
· Spreading redness or red streaks moving upward from the wound.
· Increased swelling and throbbing pain.
· Foul-smelling, thick discharge.
· Fever or chills.
· The wound area feels hot.
· Any black or darkening tissue around the edges (possible sign of gangrene).
The Path Forward: Hope and Healing
A non-healing wound can feel defeating, but with today’s advanced wound care techniques—such as negative pressure wound therapy, specialized dressings, and biologic skin substitutes—even long-standing wounds can often be closed.
Your takeaway message: A wound that won’t heal is not a personal failure; it’s a symptom. Listen to what your body is telling you. By partnering with a wound care specialist to uncover and treat the underlying cause, you can break the cycle of delayed healing and move toward recovery and restored health.
FAQs
Q1: How long is “too long” for a wound to heal? When should I officially worry?
A: As a general rule:
· Minor cuts/scrapes: Should show signs of improvement (less redness, shrinking size, forming a scab) within 1-2 weeks.
· Surgical incisions: Should be closed and well-approximated within 2-3 weeks.
· The “4-Week Rule”: If a wound has shown no measurable progress (it hasn’t gotten smaller, less red, or produced less drainage) in 4 weeks, it is considered a chronic, non-healing wound and requires medical evaluation. Don’t wait that long if there’s pain, spreading redness, or foul smell.
Q2: Is it better to let a wound “air out” or keep it covered?
A: Keep it covered with an appropriate dressing. The outdated notion that wounds need to “breathe” and scab over has been replaced by Moist Wound Healing theory. A covered, moist environment:
· Promotes faster cell migration and tissue growth.
· Reduces pain.
· Creates a barrier against bacteria.
· Prevents the wound from drying out and forming a hard scab, which actually slows healing. Change the dressing as directed, but keep it covered.
Q3: What’s the difference between a normal scab and a sign of poor healing?
A: A healthy scab is a temporary, protective cover that forms over a superficial wound and falls off on its own as new skin forms underneath.
Signs a scab indicates trouble:
· The wound underneath the scab is getting larger, more painful, or more red around the edges.
· The scab is very thick, cracked, and oozing pus (yellow/green fluid).
· The scab has been there for many weeks with no sign of new skin forming beneath it. In chronic wounds, a hard, black layer (eschar) can form, which is dead tissue that must be professionally removed (debrided) for healing to proceed.
Q4: I have diabetes. What specific steps should I take to prevent foot wounds from becoming chronic?
A: This requires a vigilant daily routine:
1. Daily Inspection: Check the tops, bottoms, sides, and between toes of both feet every single day. Use a mirror if needed.
2. Never Go Barefoot: Even indoors.
3. Proper Footwear: Wear well-fitted, protective shoes and always check inside them for pebbles or rough spots before putting them on.
4. Professional Care: See a podiatrist regularly for nail and callus care—never try to cut them yourself.
5. Manage Your Numbers: Tightly control blood sugar levels; this is the most critical factor for healing.
6. Immediate Action: Contact your doctor at the first sign of any break in the skin, redness, or swelling.
Q5: Can poor nutrition really stop a wound from healing? What should I eat?
A: Absolutely. Your body needs specific building blocks to repair tissue.
· Protein: The most critical component. Think of it as the bricks for rebuilding. Eat lean meats, fish, eggs, beans, and dairy.
· Vitamin C: Essential for forming collagen, the structural protein of skin. Found in citrus fruits, bell peppers, strawberries, and broccoli.
· Zinc: Supports immune function and cell growth. Found in seafood, nuts, seeds, and whole grains.
If you can’t eat enough, talk to your doctor about nutritional supplements like Ensure or Juven, which are formulated for wound healing.
Q6: Why do wound care specialists often remove scabs or dead tissue from a wound? Won’t that make it worse?
A: This process is called debridement, and it’s a cornerstone of chronic wound care. Dead tissue (called slough or eschar) is a physical barrier to healing and a breeding ground for bacteria. Removing it:
· Stimulates the wound bed to start generating new, healthy tissue.
· Reduces infection risk.
· Allows doctors to see the true size and depth of the wound.
It is a controlled, therapeutic procedure that promotes healing, even though it may seem counterintuitive.
Q7: My wound is clean and cared for but still not closing. What advanced treatments are available?
A: If standard care isn’t working, a Wound Care Center can offer advanced options:
· Negative Pressure Wound Therapy (NPWT): A sealed dressing connected to a pump that applies gentle suction, reducing swelling and drawing the wound edges together.
· Bioengineered Skin Substitutes: These are grafts or dressings made from human cells or collagen that provide a scaffold for new skin to grow.
· Hyperbaric Oxygen Therapy (HBOT): You breathe pure oxygen in a pressurized chamber, which dramatically increases oxygen in your blood to promote healing and fight infection.
· Growth Factor Therapy: Gels or dressings that deliver concentrated healing proteins directly to the wound.
Q8: How does smoking specifically affect wound healing?
A: Smoking is one of the most significant lifestyle factors that delays healing. Nicotine causes blood vessels to constrict (narrow), drastically reducing blood flow and the delivery of oxygen and nutrients to the wound site. It also impairs the immune system. Even cutting back during the healing process can make a measurable difference.
Q9: Is a little bit of clear drainage from a wound normal?
A: Yes, a small amount of clear or slightly yellow-pink drainage (called serous or serosanguinous fluid) is normal in the inflammatory and proliferative stages. It’s a sign your body is working. Abnormal drainage is:
· Thick, green, or yellow (purulent), indicating infection.
· Foul-smelling.
· Increasing in amount significantly.
· Bloody (bright red) if it’s not immediately after an injury.
Q10: Can stress really slow down how I heal from a cut?
A: Yes, chronic stress has a documented physiological impact on healing. High levels of the stress hormone cortisol:
· Suppress the immune system, increasing infection risk.
· Reduce inflammation, which sounds good but is actually disruptive to the crucial early healing phase.
· Can lead to poor sleep and nutrition, further hindering recovery. Managing stress through relaxation techniques is part of holistic wound care.
Q11: Should I be exercising if I have a chronic wound?
A: This depends entirely on the wound’s location and cause. Always follow your doctor’s advice.
· For leg wounds with poor circulation: Walking is often prescribed to improve blood flow (unless you have severe pain at rest).
· For pressure wounds: Exercise is not the focus; offloading pressure is.
· General Rule: Avoid activities that directly stretch, impact, or put pressure on the wound site. Ask your care team for safe, approved exercises.
Q12: When is a non-healing wound a sign of something more serious, like cancer?
A: Very rarely, a wound that won’t heal can be a sign of skin cancer, such as a basal cell carcinoma or squamous cell carcinoma that presents as an ulcer. This is why medical evaluation is critical. A doctor will biopsy any wound that:
· Has unusual, raised, or rolled edges.
· Grows steadily despite proper care.
· Is in a sun-exposed area and has been present for months.
· Bleeds very easily. A biopsy is a simple procedure to rule this out.