Ever had a “gut-wrenching” experience? Felt “butterflies” in your stomach? These common phrases hint at a profound biological truth we’ve intuitively understood for centuries: our gut and our brain are deeply linked. But this connection is more than just poetic language—it’s a sophisticated, two-way communication network called the gut-brain axis, and it’s revolutionizing our understanding of mental health.
The food you eat doesn’t just build your body; it fundamentally shapes your mind. Let’s explore the fascinating science behind this connection and how you can harness it to support your mental wellness.
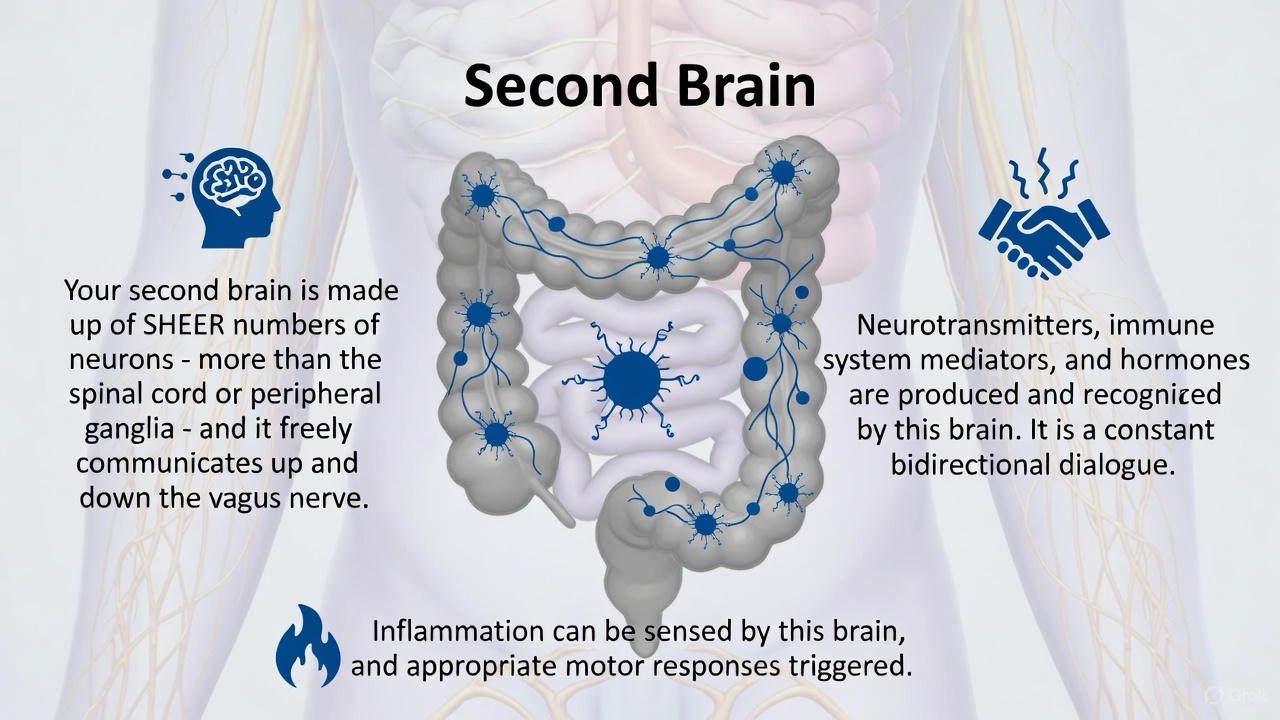
Your Gut: The “Second Brain” Explained
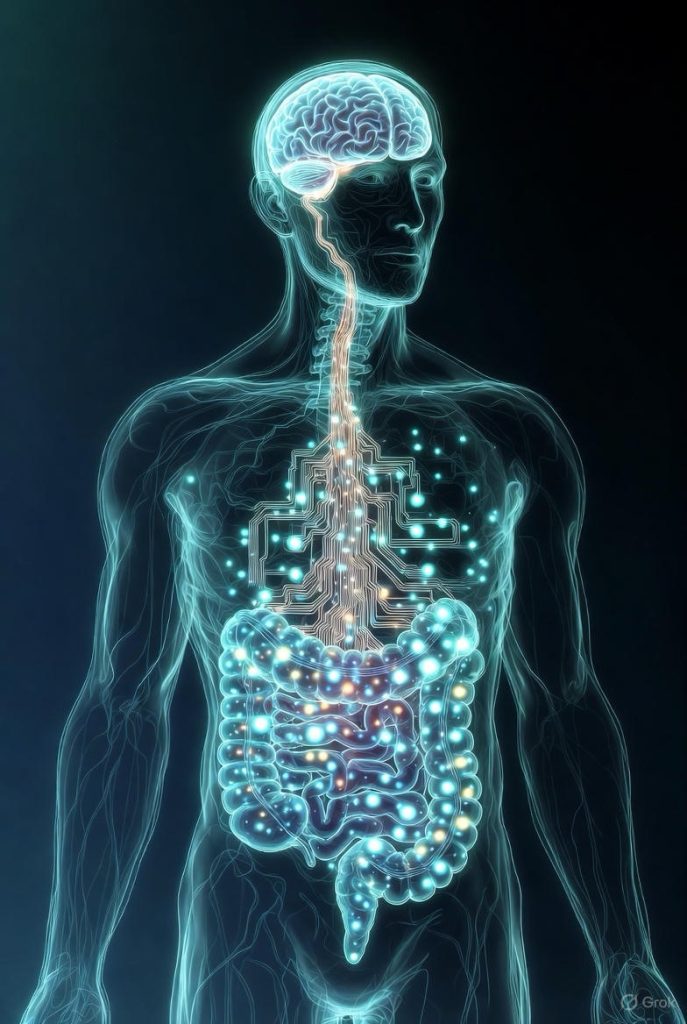
Your digestive system houses its own independent nervous system, called the enteric nervous system (ENS), often dubbed the “second brain.” This vast network of over 100 million nerve cells lines your gastrointestinal tract from esophagus to rectum. It’s in constant conversation with the brain in your head via a massive nerve highway called the vagus nerve.
But the key players in this conversation are the trillions of bacteria, fungi, and other microbes that live in your gut, collectively known as your gut microbiome. Think of this community as a bustling city within you. A healthy, diverse microbiome is like a well-functioning city where everyone contributes to peace and prosperity. An unbalanced one (called dysbiosis) is like a city in chaos, leading to inflammation and trouble.
The Science of the Conversation: How Your Gut Talks to Your Brain
So, how does a bacterium in your colon affect the emotions in your mind? It uses several powerful channels:
1. Neurotransmitter Production:
You might think serotonin, the famous “happy chemical,” is made only in the brain. But shockingly, an estimated 90% of your body’s serotonin is produced in your gut by certain microbes. Other gut bacteria also produce GABA (a calming neurotransmitter) and dopamine (involved in motivation and pleasure). Your gut flora directly influences the production of these critical mood regulators.
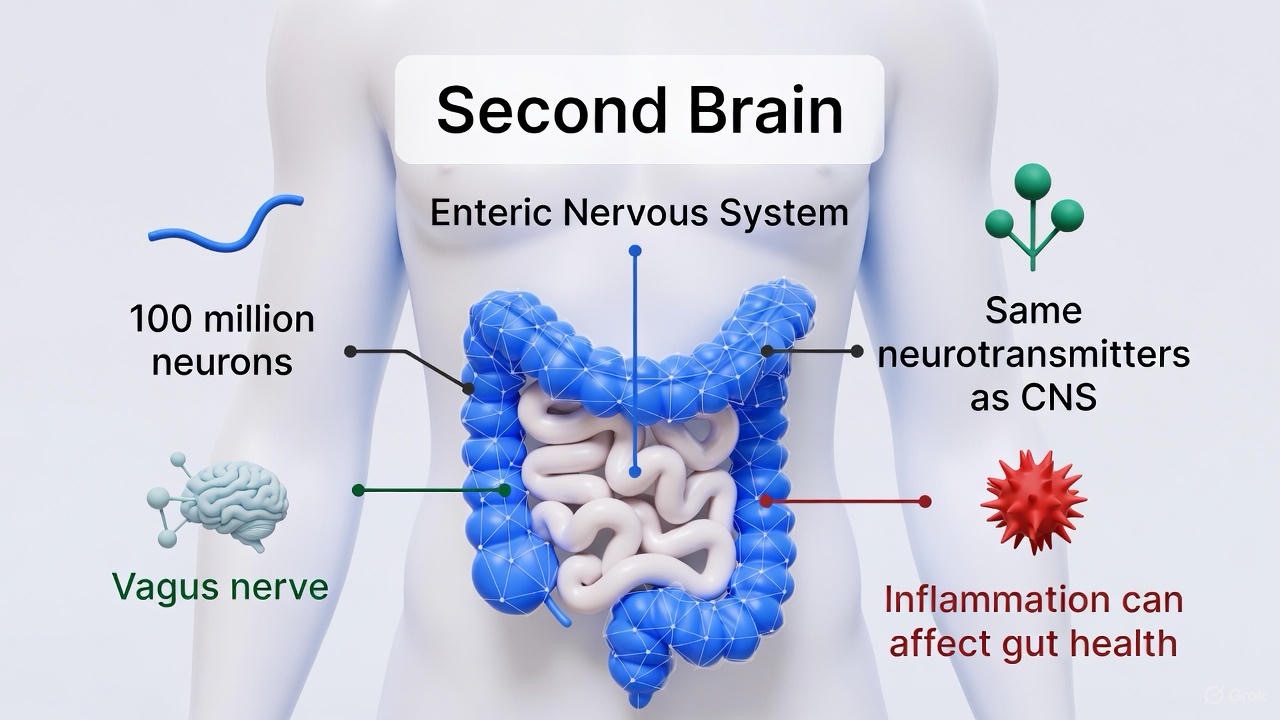
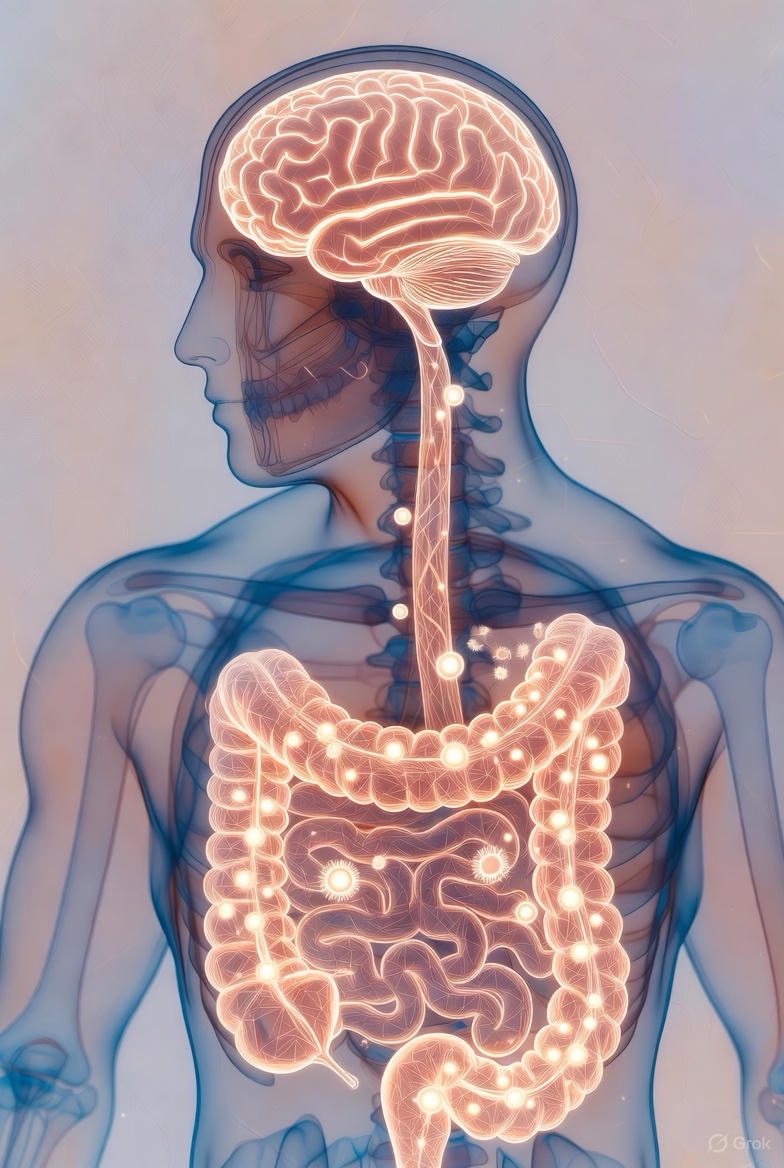
2. The Vagus Nerve Superhighway:
This is the direct phone line between your gut and brain. Gut microbes stimulate the vagus nerve, sending signals that can influence brain regions responsible for mood, anxiety, and stress response. A healthy gut sends “all is well” signals, while an inflamed gut can send distress signals that contribute to feelings of anxiety.
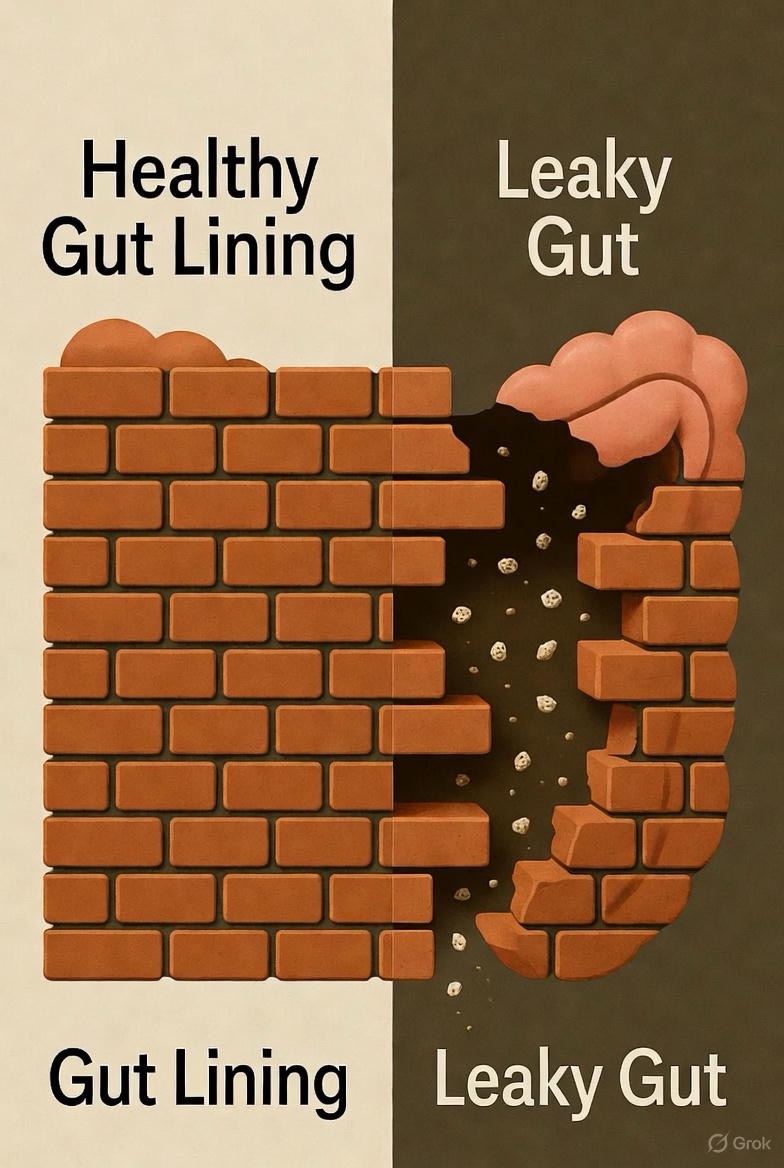
3. Systemic Inflammation:
An unhealthy gut microbiome, often from a poor diet, can damage the delicate lining of the intestines. This leads to “leaky gut,” where toxins and food particles seep into the bloodstream. The body’s immune system responds with chronic, low-grade inflammation. This inflammation can travel throughout the body and cross the blood-brain barrier, which is strongly linked to the development of depression and anxiety.
4. Short-Chain Fatty Acids (SCFAs):
When your good gut bacteria feast on dietary fiber, they produce beneficial compounds called Short-Chain Fatty Acids (like butyrate). SCFAs are powerhouse molecules that strengthen the gut barrier, reduce inflammation, and may even help protect the brain itself.
Dietary Tips to Feed Your Mind by Feeding Your Gut
The most powerful part of this science is that it’s actionable. You can directly influence this complex system through the food you eat. Here’s how to cultivate a microbiome that supports mental wellness.
1. Feed the Good Guys: Eat a Diverse Range of Fiber
Fiber from plants is the preferred food for your beneficial gut bacteria. You can’t digest it, but they can, and they thrive on it.
· What to do: Aim for 30+ different plant foods per week. This doesn’t just mean fruits and vegetables. Count nuts, seeds, legumes (beans, lentils), whole grains, herbs, and spices.
· Simple swaps: Add a tablespoon of mixed seeds (chia, flax, pumpkin) to your yogurt or oatmeal. Snack on a handful of almonds and berries. Add a can of mixed beans to your soup.
2. Embrace Fermented Foods: Your Source of Probiotics

Probiotics are live, beneficial bacteria that can take up temporary residence in your gut and add to its diversity.
· What to do: Incorporate one or two servings of fermented foods into your daily diet.
· Options to try: Plain yogurt, kefir, unpasteurized sauerkraut, kimchi, kombucha, and miso. Check the label for “live and active cultures.”
3. Nourish with Prebiotics: The Fertilizer for Your Gut Garden

Prebiotics are specific types of fiber that act as fertilizer, selectively stimulating the growth of your good bacteria.
· What to do: Include prebiotic-rich foods in your meals.
· Top sources: Garlic, onions, leeks, asparagus, bananas, oats, apples, and Jerusalem artichokes.
4. Limit the Party Crashers: Sugar and Ultra-Processed Foods
A diet high in sugar and unhealthy fats (common in processed foods) does two things: it feeds the less desirable, harmful bacteria and yeast, and it actively reduces the diversity of your good gut microbes, promoting inflammation.
· What to do: Be mindful of sugary drinks, sweets, refined white breads, and processed snacks. Think of these as “party crashers” that disrupt the peaceful, productive city in your gut.
You Are What Your Bacteria Eat
The connection between your plate and your mental state is one of the most exciting frontiers in wellness. By making conscious choices to feed your gut microbiome a diverse, fiber-rich diet, you are not just nurturing your body—you are sending direct signals of calm and stability to your brain.
Start small. Add one extra vegetable to your dinner. Try a new fermented food this week. Each positive choice is a step toward a happier, healthier gut, and a more resilient mind.

FAQs
Q1: This sounds promising, but is this link between gut and mental health really proven?
A: Yes, the gut-brain axis is a well-established scientific concept in neurogastroenterology. While it’s a rapidly evolving field, numerous studies in humans and animals show a strong correlation. For instance, researchers have found that people with certain psychological disorders often have different gut microbiome compositions than healthy individuals. Furthermore, studies where probiotics are given to humans (clinical trials) have shown measurable reductions in stress, anxiety, and symptoms of depression compared to placebo groups.
Q2: How fast can changing my diet actually impact my mood?
A: It’s not an overnight fix like a medication, but it’s also not a years-long process. Many people report noticing subtle changes, such as improved energy levels, less “brain fog,” and a more stable mood, within a few weeks of making consistent dietary changes. For more significant and measurable shifts in microbiome diversity and mental well-being, think in terms of several months of sustained healthy eating. Consistency is key.

Q3: If most serotonin is in my gut, why don’t I feel happy in my stomach?
A: This is a brilliant question. The serotonin produced in your gut primarily acts locally within the digestive system. It regulates gut movements, blood flow, and other digestive processes. It cannot cross the blood-brain barrier to enter your brain. However, it influences your brain indirectly by:
1. Producing other chemicals that can cross the barrier.
2. Sending signals via the vagus nerve.
3. Controlling systemic inflammation that affects the entire body, including the brain.
So, gut serotonin is crucial for creating a healthy internal environment that allows your brain to regulate its own mood effectively.
Q4: Should I just take a probiotic supplement instead of changing my diet?
A: Probiotic supplements can be a helpful addition, but they are not a replacement for a healthy diet. Think of it this way:
· Probiotics (supplements/fermented foods) = Adding new good citizens to your gut city.
· Prebiotics (fiber-rich diet) = Providing the food and infrastructure to help all the good citizens thrive.
If you only add new citizens but don’t feed them (with prebiotics), they won’t stay for long. A diverse diet ensures your entire microbial ecosystem flourishes.

Q5: What should I look for in a probiotic supplement for mental health?
A: Look for strains that have been studied specifically for mood. The most researched genera for mental health (often called “psychobiotics”) are Lactobacillus and Bifidobacterium. Look for a supplement that:
· Lists specific strains (e.g., Lactobacillus helveticus, Bifidobacterium longum).
· Guarantees a high number of live cultures (CFUs) at the time of expiration, not just manufacture.
· Is backed by third-party testing for quality.
Always consult with your doctor or a registered dietitian before starting a supplement, as strains matter for different goals.

Q6: I can’t eat 30 different plants a week. Is there a simpler place to start?
A: Absolutely! The “30 plants” goal is a fantastic target for maximum diversity, but it can be overwhelming. A much simpler and highly effective starting point is:
· Focus on Fiber: Aim for 25-35 grams of fiber per day. Read labels and choose high-fiber foods.
· Add One Prebiotic Food Daily: Make a conscious effort to include one thing from this list every day: a banana, some onions/garlic in your cooking, oats for breakfast, or a handful of almonds.
· “Eat the Rainbow”: Simply try to include fruits and vegetables of different colors throughout your day. This is an easy way to automatically increase diversity.

Q7: Are there any specific foods I should avoid for my mental health?
A: The evidence points most strongly to the negative impact of highly processed foods. These are typically high in:
· Refined Sugars & Carbs: Feed harmful bacteria and promote inflammation.
· Unhealthy Fats: (e.g., high levels of omega-6 from processed vegetable oils) can contribute to brain inflammation.
· Artificial Sweeteners: Some studies suggest sweeteners like aspartame and saccharin may negatively alter the gut microbiome.
The goal isn’t perfection, but rather to gradually shift the balance so that whole, fiber-rich foods make up the bulk of your diet.

Q8: What about alcohol and caffeine?
A:· Alcohol: In excess, alcohol is directly harmful to the gut lining and can disrupt the microbiome balance, promoting inflammation. Moderate consumption is key.
· Caffeine: For most people, moderate coffee consumption (2-3 cups) may actually be beneficial for the gut microbiome due to its polyphenols. However, it can exacerbate anxiety and digestive issues in sensitive individuals. Listen to your body.
Q9: Can improving my gut health help with my anxiety?
A: Yes, it is one of the most promising lifestyle approaches for managing anxiety. Since the vagus nerve is a direct line from the gut to the brain, a calm, healthy gut can send “calm” signals, reducing the physiological state of anxiety. Reducing gut-based inflammation also helps lower overall systemic stress on the body. It’s a powerful complementary strategy alongside other treatments like therapy.
Q10: I have IBS. Does this mean my mental health is at risk?
A: There is a very high comorbidity (conditions occurring together) between IBS and mood disorders like anxiety and depression. This is a classic example of the gut-brain axis in dysfunction. The chronic gut inflammation and discomfort of IBS can worsen mental health, and conversely, stress and anxiety can trigger or worsen IBS symptoms. Treating both the gut and the mind together is often the most effective approach for IBS sufferers.
Q11: I’m on an antidepressant (SSRI). Can diet changes interfere?
A: A healthy diet will not “interfere” with the medication’s mechanism. In fact, it may help support its effectiveness by improving your overall health and reducing inflammation. However, you should never stop or change your medication based on dietary changes. Always work with your prescribing doctor. Think of diet as a foundational support that works alongside your medical treatment.