Have you ever noticed a persistent, painful sore on someone’s lower leg, often near the ankle, that just doesn’t seem to heal? This could be a venous stasis ulcer—a common but often misunderstood condition that affects millions of people worldwide. In this article, we’ll break down what venous stasis ulcers are, their symptoms, underlying causes, and the treatment options available to manage and heal them.
What Are Venous Stasis Ulcers?
Venous stasis ulcers, also known as venous leg ulcers, are open wounds that typically occur on the lower leg or ankle. They are the most common type of leg ulcer, accounting for about 80–90% of cases. These ulcers develop due to poor circulation in the venous system, specifically when veins in the legs fail to efficiently return blood back to the heart—a condition known as venous insufficiency.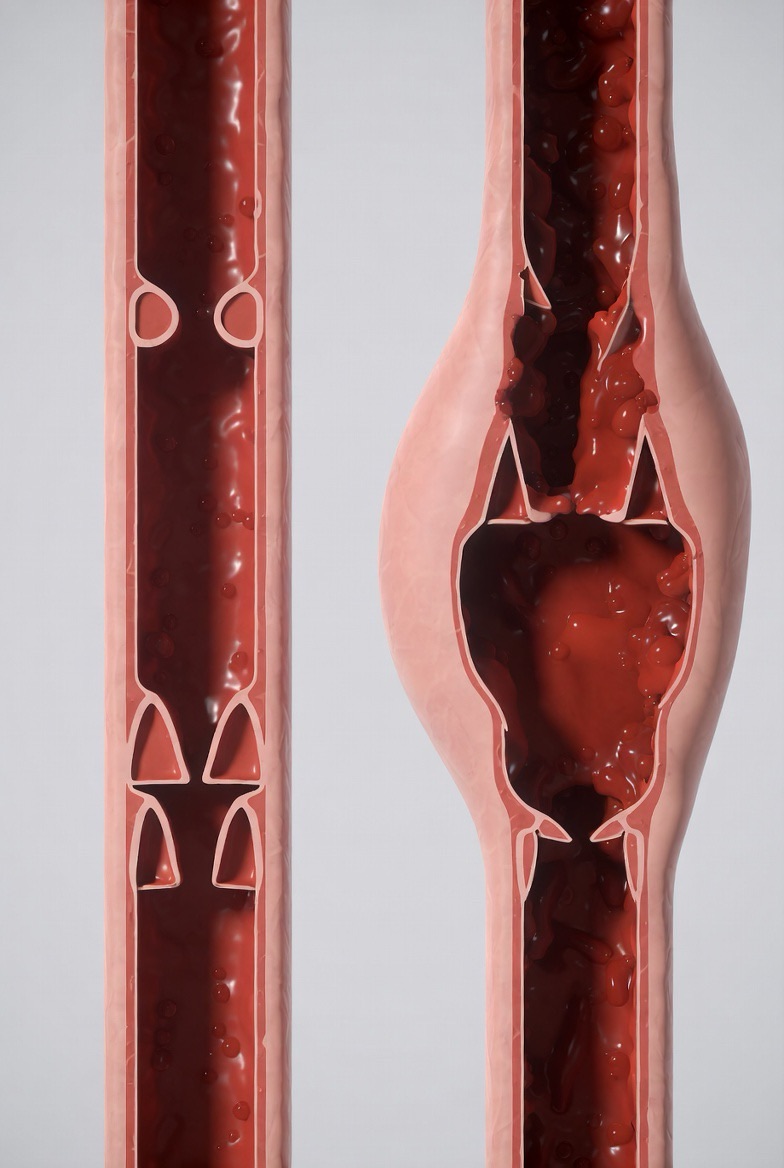
Recognizing the Symptoms
Early detection is crucial for effective management. Here are common symptoms to watch for:
· Location: Usually found on the inner side of the leg, just above the ankle.
· Appearance: A shallow sore with irregular edges, often surrounded by discolored, swollen, or hardened skin.
· Skin Changes: The surrounding skin may appear reddish-brown, shiny, tight, or warm to the touch.
· Discharge: The ulcer may weep clear fluid or pus if infected.
· Pain and Swelling: Aching, heaviness, or swelling in the legs, especially after prolonged standing.
· Itching and Burning: The affected area may feel itchy or have a burning sensation.
If you notice any of these signs, it’s important to consult a healthcare professional for a proper diagnosis.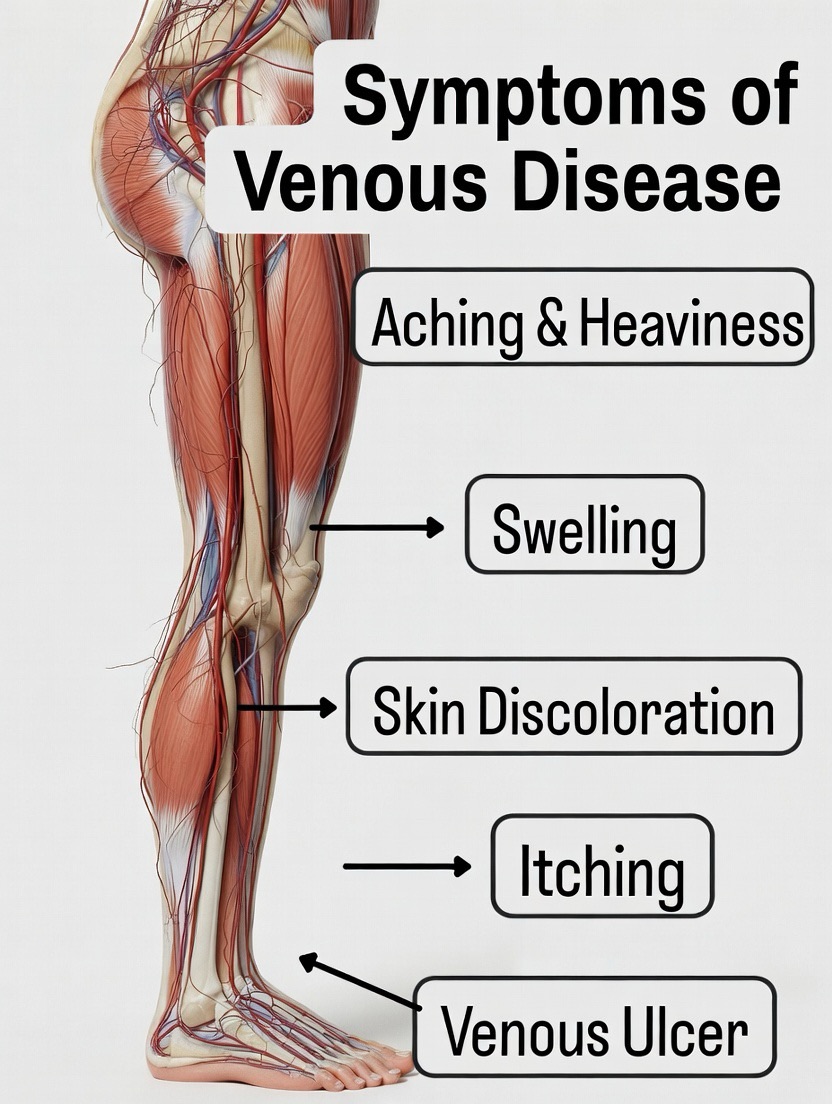
Root Causes: Why Do They Develop?
Venous stasis ulcers don’t appear overnight. They are usually the result of long-standing venous insufficiency. Here’s a breakdown of the key causes:
1. Venous Insufficiency:
Damaged or weakened valves in the leg veins allow blood to flow backward and pool in the lower legs. This increased pressure (venous hypertension) weakens the skin and tissues, making them prone to ulcers.
2. Deep Vein Thrombosis (DVT):
A history of blood clots can damage vein valves and lead to chronic venous insufficiency.
3. Varicose Veins:
Enlarged, twisted veins contribute to poor circulation.
4. Other Risk Factors:
· Age (more common in older adults)
· Obesity
· Sedentary lifestyle or prolonged standing
· Previous leg injuries or surgeries
· Family history of venous issues
· Smoking
Treatment Options: Pathways to Healing
While venous stasis ulcers can be stubborn, effective treatment plans can promote healing and prevent recurrence. Treatment is typically multi-faceted:
1. Compression Therapy
· The cornerstone of treatment. Compression bandages or stockings improve circulation by helping veins move blood upward, reducing swelling and promoting healing.
· Important: Compression should only be applied under medical supervision after assessing arterial blood flow.
2. Wound Care
· Cleaning and Dressing: Keeping the ulcer clean and covered with appropriate dressings (like hydrocolloids or foam dressings) to maintain a moist healing environment and protect from infection.
· Debridement: Removal of dead tissue to encourage new tissue growth.
3. Medications
· Topical: Antibiotic ointments if infection is present.
· Oral: Antibiotics for active infection, or medications to improve blood flow in some cases.
· Pain Management: Over-the-counter or prescribed pain relievers.
4. Lifestyle and Home Care
· Elevation: Elevating legs above heart level several times a day reduces swelling.
· Exercise: Regular walking and leg exercises boost calf muscle pump action, aiding circulation.
· Skin Care: Keeping skin moisturized and protecting it from injury.
5. Advanced Interventions
· Endovenous Ablation or Sclerotherapy: Procedures to treat underlying varicose veins or faulty veins.
· Skin Grafting: For large or non-healing ulcers, grafting healthy skin can aid recovery.
· Negative Pressure Wound Therapy: Uses a vacuum device to promote healing in stubborn wounds.
6. Preventing Recurrence
· Even after healing, lifelong management is key. Continued use of compression stockings, maintaining a healthy weight, staying active, and regular skin checks can prevent new ulcers from forming.
When to Seek Help
If you suspect a venous ulcer, don’t delay medical attention. Untreated ulcers can lead to complications like severe infections (cellulitis), bone infections (osteomyelitis), or permanent skin changes. A healthcare provider—often a dermatologist, vascular specialist, or wound care nurse—can provide a tailored treatment plan.
The Takeaway
Venous stasis ulcers are a chronic condition rooted in circulatory issues, but they are manageable. With proper treatment, most ulcers heal within a few months. Understanding the symptoms, causes, and treatments empowers patients and caregivers to take proactive steps toward healing and long-term leg health.
If you or a loved one is dealing with a non-healing leg wound, remember: you’re not alone, and effective help is available. Start the conversation with a healthcare professional today—it’s the first step on the path to recovery.
FAQs
Q1: How do I know if my leg wound is a venous ulcer or something else?
A: Venous ulcers have specific characteristics: they’re usually shallow with irregular edges, located on the inner lower leg or ankle, and surrounded by discolored (reddish-brown), tight, or swollen skin. The leg often feels heavy or achy. Other ulcers, like arterial ulcers (due to poor blood inflow), are typically deeper, appear on the feet or toes, and are extremely painful. A doctor can perform a simple ankle-brachial index (ABI) test to check your blood circulation and provide a definitive diagnosis. Never self-diagnose—proper assessment is crucial.
Q2: Can venous ulcers heal on their own without treatment?
A: It is very rare for a venous ulcer to heal completely without proper treatment. Because the root cause is underlying venous insufficiency (faulty circulation), the body’s natural healing process is severely impaired. Without treatment, ulcers often get larger, become more painful, and risk serious infection. Professional medical care is essential to address the circulation problem and create the right environment for healing.
Q3: Is compression therapy painful? Is it always necessary?
A: Compression might feel tight or unusual at first, but it should not be painful. Properly applied medical-grade compression is the single most effective treatment for venous ulcers. It counteracts the venous pressure that causes the ulcer. However, compression must not be used if you also have significant arterial disease. Your doctor will test for this first. The type and strength of compression (bandages vs. stockings) will be tailored to your specific needs.
Q4: How long does it take for a venous stasis ulcer to heal?
A: Healing is a process, not an overnight event. With consistent, proper treatment (especially compression), a typical venous ulcer may show improvement in a few weeks and can take 3 to 6 months to heal completely. Larger, older, or infected ulcers may take longer. The key factors for healing are adhering to the treatment plan, managing underlying conditions, and preventing new injuries to the area.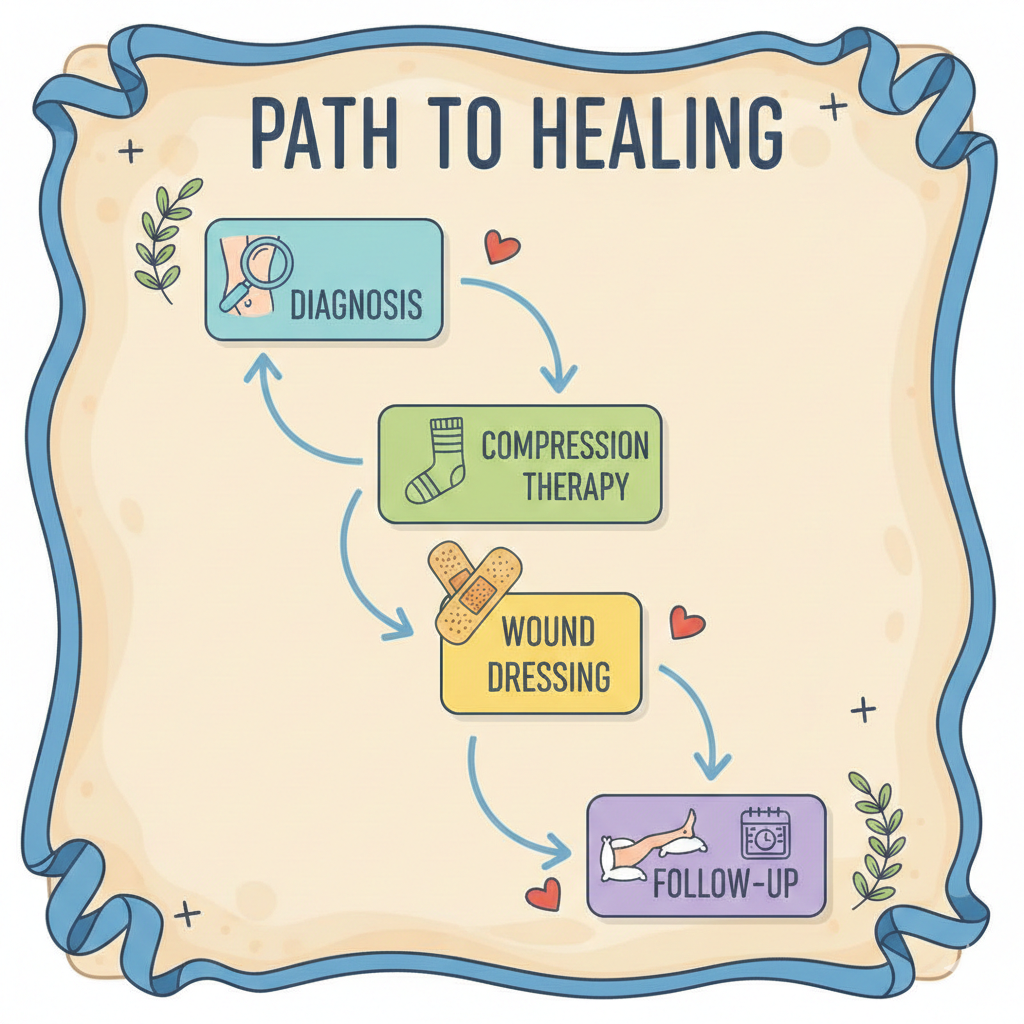
Q5: What can I do at home to help the ulcer heal faster?
A: You play a vital role in your own healing:
· Elevate: Raise your legs above your heart level whenever you’re sitting or lying down.
· Stay Active: Walk regularly. The calf muscle acts as a pump to help push blood upward.
· Follow Wound Care: Change dressings as instructed and keep the surrounding skin clean and moisturized (but not the ulcer itself unless directed).
· Wear Compression: Use your prescribed stockings or bandages exactly as told.
· Eat Well: A balanced diet rich in protein, vitamin C, and zinc supports tissue repair.
Q6: Can venous ulcers come back after they’ve healed?
A: Yes, the risk of recurrence is high—up to 70%—because the underlying venous insufficiency is a chronic, lifelong condition. Prevention is permanent management. This almost always includes:
· Wearing prescription compression stockings daily.
· Continuing leg elevation and exercise.
· Moisturizing skin to prevent cracking.
· Regular check-ups with your doctor.
Think of healing the ulcer as “phase one”; ongoing prevention is “phase two” for life.
Q7: Are venous ulcers a sign of diabetes?
A: Not directly. Venous ulcers are caused by problems in the veins. Diabetes primarily affects arteries and nerves, which can lead to different types of ulcers (neuropathic or arterial). However, a person can have both diabetes and venous disease, which complicates healing. It’s important for your healthcare team to know about all your health conditions.
Q8: What happens if a venous ulcer gets infected?
A: Signs of infection include increased pain, redness spreading from the wound, swelling, warmth, foul-smelling discharge, or fever. An infected ulcer is a serious complication that can lead to cellulitis (deep skin infection), bone infection, or sepsis. Contact your doctor immediately if you suspect infection. Treatment usually involves oral or intravenous antibiotics and more frequent wound care.
Q9: I have varicose veins. Am I going to get an ulcer?
A: Having varicose veins increases your risk, as they are a sign of venous insufficiency. However, not everyone with varicose veins develops an ulcer. You can significantly lower your risk by managing your vein health: wear compression stockings if recommended, maintain a healthy weight, exercise, avoid prolonged standing/sitting, and protect your legs from injury. If you notice skin changes like darkening or hardening around your ankles, see a vascular specialist.
Q10: Who should I see for treatment?
A: Start with your primary care physician. They will often coordinate care with specialists, which may include:
· A Vascular Specialist: For diagnosing and treating the underlying vein problems.
· A Wound Care Clinic/Nurse: Experts in advanced dressings and healing techniques.
· A Dermatologist: For skin-related complications.
A team approach usually yields the best results.

