Imagine a home security system designed to protect you, but one day it malfunctions—locking you out, setting off false alarms, and even damaging your own house. This, in essence, is what happens in an autoimmune disease. The body’s sophisticated defense network—the immune system—mistakenly targets its own healthy cells, tissues, and organs.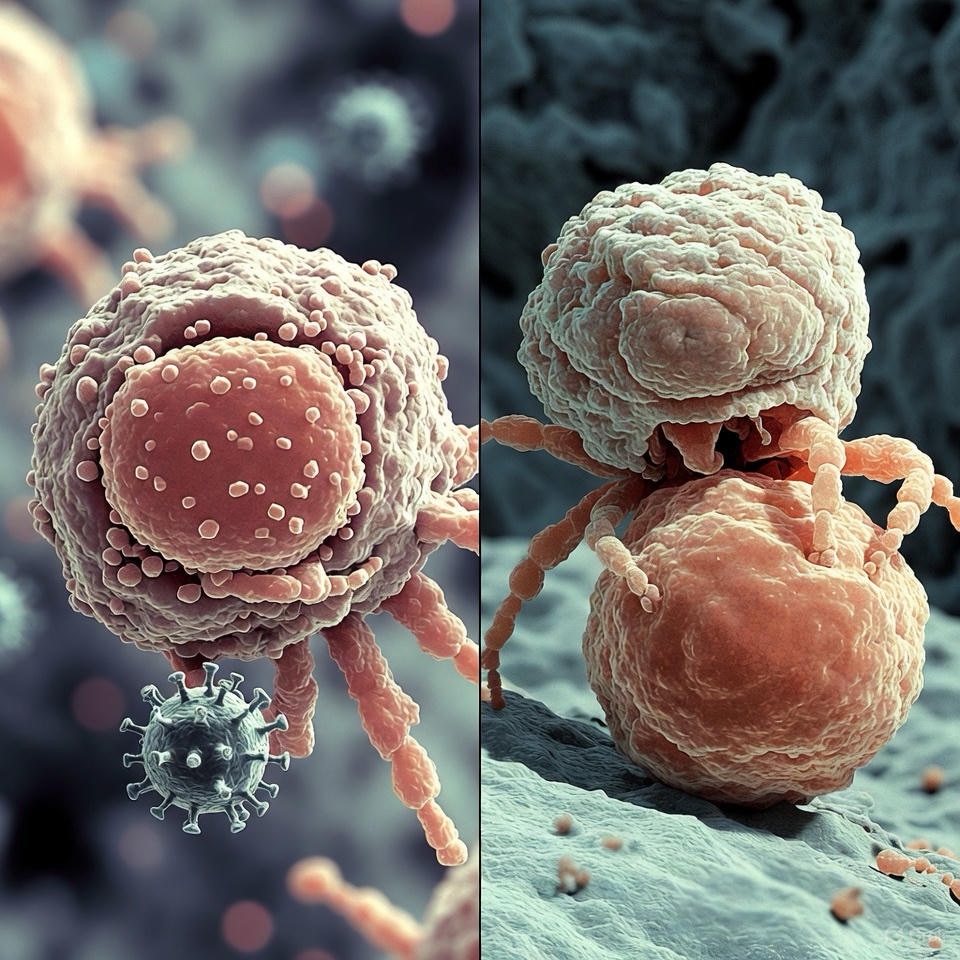
It’s a complex and often misunderstood category of illness, affecting approximately 1 in 10 people, with women disproportionately impacted. By understanding the “why” and recognizing early signs, we can move from fear to informed action.
Why Does the Body Turn on Itself?
The precise cause of autoimmune diseases remains one of immunology’s great puzzles. Researchers believe it’s rarely one single factor, but rather a “perfect storm” of elements:
· Genetics: A family history can increase susceptibility. You might inherit a tendency for the immune system to react, but it often requires other triggers.
· Environmental Triggers: Infections (viruses or bacteria), certain medications, or exposure to chemicals can act as a match, igniting an autoimmune response in those predisposed.
· Hormones: Many autoimmune diseases are more common in women, suggesting sex hormones may play a role in modulating immune responses.
· The “Hygiene Hypothesis”: Some theories suggest that living in overly clean environments may prevent our immune systems from learning to properly distinguish between real threats and the body’s own cells.
· Leaky Gut: Emerging research explores the link between intestinal permeability and autoimmunity, where particles escaping from the gut may trigger an immune reaction.
In short, it’s believed a person with a genetic predisposition encounters an environmental trigger, leading the immune system to lose its ability to distinguish “self” from “non-self.” This results in chronic inflammation and damage to whatever part of the body is under attack—be it joints, skin, thyroid, nerves, or internal organs.
Common Early Signs: Listening to Your Body’s Alarms
Autoimmune diseases are masters of disguise, and their early symptoms are often vague, overlapping, and easily dismissed as everyday fatigue or stress. This is why awareness is so crucial. If you experience a constellation of the following symptoms persistently and without clear cause, it’s worth a conversation with your doctor.
1. Overwhelming Fatigue
This isn’t just feeling tired after a long day. It’s a profound, unshakeable exhaustion that isn’t relieved by sleep and significantly interferes with daily life.
2. Low-Grade Fever and Malaise
Frequent, unexplained low-grade fevers or a constant feeling of being “unwell” or “coming down with something” are common early flags.
3. Muscle and Joint Pain
Stiffness, aches, and pain in muscles and joints—especially morning stiffness that lasts more than 30 minutes—can be early signs of conditions like rheumatoid arthritis or lupus.
4. Skin Changes and Rashes
Unexplained rashes, sun-sensitive redness (like the classic butterfly rash across the cheeks in lupus), or changes in skin texture and color should not be ignored.
5. Swelling and Redness
Localized swelling, redness, or warmth in joints, or unexplained swelling in other areas, points to underlying inflammation.
6. “Brain Fog”
Difficulty concentrating, memory lapses, and a general feeling of mental cloudiness are frequently reported by patients long before a diagnosis.
7. Hair Loss or Changes
Patchy or significant hair loss beyond normal shedding can be a sign of conditions like alopecia areata or lupus.
8. Numbness and Tingling
A “pins and needles” sensation in the hands and feet can indicate nerve involvement, as seen in diseases like multiple sclerosis.
9. Digestive Upset
Ongoing abdominal pain, bloating, diarrhea, or constipation may signal autoimmune issues targeting the gut, such as Crohn’s disease or celiac disease.
10. Weight Changes or Temperature Sensitivity
Unexplained weight gain or loss, or a new intolerance to heat or cold, can point to autoimmune thyroid diseases like Hashimoto’s or Graves’.
The Path Forward: From Symptoms to Care
If you see yourself in several of these signs, don’t panic—but do take action.
1. Document Your Symptoms: Keep a detailed journal of what you’re experiencing, when it happens, and its severity. This is invaluable for your doctor.
2. Find the Right Doctor: Start with your primary care physician. Be persistent and descriptive. A referral to a rheumatologist (a specialist in autoimmune and inflammatory diseases) is often the next step.
3. Prepare for a Process: Diagnosing autoimmune diseases can be challenging. It often involves a combination of physical exams, detailed personal and family history, blood tests (like antinuclear antibody tests), and imaging studies. Be patient with the process.
4. Embrace a Proactive Partnership: Treatment focuses on managing symptoms, reducing inflammation, and suppressing the overactive immune response. This often involves medications, lifestyle changes (like anti-inflammatory nutrition, stress management, and gentle exercise), and a strong support system.
Understanding autoimmune diseases demystifies the body’s complex rebellion. By recognizing the early whispers of symptoms, you empower yourself to seek answers and advocate for your health. Remember, you are not your diagnosis—but understanding it is the first powerful step toward managing it and living a full, vibrant life.
FAQs
1. Is an autoimmune disease the same as being immunocompromised?
Answer: Not exactly, and this is a key distinction.
· Autoimmune Disease: Your immune system is overactive and misguided. It attacks your own body but is not necessarily weak.
· Immunocompromised: Your immune system is underactive or weakened, making it harder to fight off infections.
· Important Note: Many treatments for autoimmune diseases (like immunosuppressant drugs) work by deliberately suppressing the overactive immune system. This can make a person immunocompromised as a side effect of treatment, even though the underlying disease involves an overactive response.
2. Can autoimmune diseases be cured?
Answer: Currently, there is no universal cure for autoimmune diseases. However, they can almost always be effectively managed. Treatment goals are to:
· Reduce symptoms (like pain and fatigue).
· Control the autoimmune response and minimize inflammation.
· Prevent further damage to organs and tissues.
With proper treatment, many people with autoimmune conditions live full, active lives. This is considered a state of remission, where the disease is quiet but not gone.
3. Are autoimmune diseases contagious?
Answer: No. You cannot “catch” an autoimmune disease from someone else. They are caused by a complex interplay of genetics and environmental factors unique to the individual.
4. Why are women more affected?
Answer: While the exact reasons are still being researched, it’s strongly linked to hormonal and genetic factors.
· Sex Hormones: Estrogen is generally immune-stimulating, while testosterone is more immunosuppressive. This hormonal difference may predispose women to an over-reactive immune response.
· Chromosomes: Women have two X chromosomes, and many immune-related genes are located on the X chromosome. Issues with X-chromosome inactivation may play a role.
· Pregnancy: The immune system undergoes complex changes during pregnancy, which can sometimes trigger or alter the course of autoimmune disease.
5. How long does it take to get a diagnosis?
Answer: Unfortunately, it can be a long and frustrating process, often taking 3 to 5 years or more from the onset of symptoms. This is because:
· Early symptoms are vague and common to many conditions.
· There is no single test for most autoimmune diseases.
· Diagnosis often requires ruling out other possibilities and seeing a pattern of symptoms and test results over time.
Patient advocacy—documenting symptoms persistently and seeking specialists—is crucial to shortening this timeline.
6. Can diet and lifestyle really help?
Answer: Yes, absolutely. While they are not a replacement for medical treatment, they are foundational to management.
· Anti-Inflammatory Diet: Focusing on whole foods (fruits, vegetables, fatty fish, nuts), reducing processed foods and sugars, and identifying personal food triggers (like gluten for some) can significantly reduce symptom flares.
· Stress Management: Chronic stress can exacerbate autoimmune responses. Practices like meditation, yoga, and adequate sleep are therapeutic.
· Gentle Exercise: Regular, low-impact activity (like walking, swimming, tai chi) reduces inflammation and combats fatigue without overtaxing the body.
Think of medication as putting out the fire, and lifestyle as removing the flammable materials.

7. If I have one autoimmune disease, will I get another?
Answer: The risk is increased. This is called polyautoimmunity. Having one autoimmune condition makes you statistically more likely to develop a second (e.g., someone with rheumatoid arthritis may later develop Sjögren’s syndrome). This is due to shared underlying genetic and immune system dysregulation.
8. Is it all in my head? Why do my symptoms come and go?
Answer: No, it is not “in your head.” The fluctuating nature is a hallmark of autoimmune diseases and is one of the most challenging aspects.
· Flare-Ups (or Flares): Periods where symptoms worsen significantly due to increased disease activity.
· Remission: Periods where symptoms lessen or disappear.
Flares can be triggered by stress, infection, hormonal changes, or environmental factors. This unpredictability is real and physical, not psychological.
9. What kind of doctor should I see?
Answer:
· Start with your Primary Care Physician (PCP): They can perform initial tests and rule out other conditions.
· Specialist Referral: You will likely be referred to a rheumatologist (for diseases like lupus, RA, Sjögren’s). Other specialists include:
· Endocrinologist (for thyroid diseases like Hashimoto’s)
· Gastroenterologist (for Crohn’s, celiac, UC)
· Neurologist (for MS)
· Dermatologist (for psoriasis, scleroderma)
10. Are my children at risk?
Answer: There is a genetic predisposition, but it’s not a direct inheritance. You can pass on a higher risk, not the disease itself. A child with a parent who has an autoimmune disease has a higher chance than the general population of developing one, but many will not. Environmental triggers still play a necessary role. Informing your pediatrician of your family history is wise for early monitoring.


