Navigating healthcare can feel overwhelming, but preventative care is one of the most powerful tools you have for a long, vibrant life. Think of it as routine maintenance for your most valuable asset: your body. This decade-by-decade checklist isn’t about fear—it’s about empowerment. By knowing what to expect and when, you can partner with your healthcare provider to stay ahead of the curve.

The Foundation: For Every Decade (20s+)
· Annual Wellness Visit: Even if you feel perfectly healthy, this is for establishing a relationship with your provider, discussing lifestyle, and updating vaccinations.
· Monthly Breast Self-Awareness: Know what’s normal for you. Report any persistent changes (lumps, skin changes, nipple discharge) to your doctor.
· Skin Check: Annual self-exams for new or changing moles. Discuss a professional dermatology screening if you have a family history of skin cancer, many moles, or significant sun exposure.
· Mental Health Check-In: Your emotional well-being is integral to your health. Discuss stress, mood, or anxiety openly with your provider.
· Dental Exam: Cleanings and check-ups every six months.
· Eye Exam: Every 2 years, or as recommended.
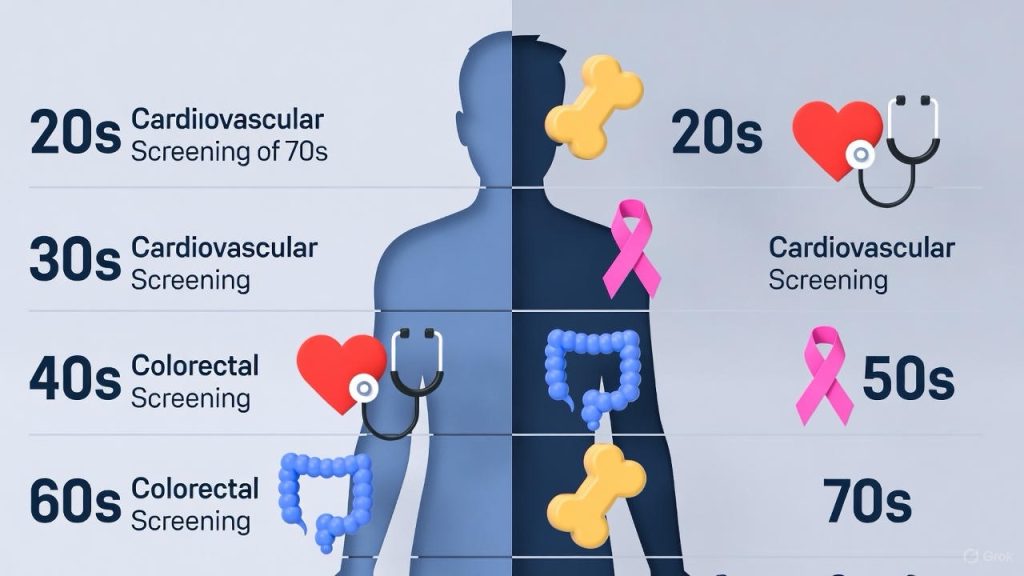
Your 20s: Building a Strong Baseline

This is the decade of establishing healthy habits and baselines for future health.
· Clinical Breast Exam: Your provider may perform one every 1-3 years.
· Pap Smear & HPV Test: Starting at age 21, a Pap smear is recommended every 3 years to screen for cervical cancer. At 25+, HPV testing (often co-tested with a Pap) may extend the interval to every 5 years. (Follow your provider’s specific guidance).
· STI Screening: Annually or with new partners, for chlamydia, gonorrhea, and HIV. Discuss your need for syphilis and hepatitis C testing.
· Blood Pressure & Basic Wellness Panel: At least every 2 years if normal. Checks cholesterol, blood sugar, and thyroid function.
· Fertility & Contraception: A prime time for open discussions about reproductive goals and options.
Your 30s: Proactive Maintenance

Life often gets busier in your 30s. Prioritizing your health screenings ensures you can keep up with your ambitions.
· Continue all screenings from your 20s.
· Cervical Cancer Screening: Continue Pap/HPV testing per guidelines (typically every 3-5 years).
· First Mammogram? If you have a family history of breast cancer (especially in a first-degree relative like a mother or sister), talk to your doctor about whether to start screening before 40.
· Fertility & Pregnancy: Preconception counseling is valuable if considering pregnancy. Continue prenatal care screenings if pregnant.
· Metabolic Health: Keep an eye on blood pressure, cholesterol, and fasting blood sugar as risks for conditions like PCOS, diabetes, and hypertension can begin to surface.
· Thyroid Function: A TSH test is often recommended, especially if experiencing fatigue, weight changes, or mood swings.
Your 40s: A Pivotal Decade for Prevention

This decade marks the start of several key screenings to catch potential issues early, when they are most treatable.
· Mammograms: The major update! Begin annual or biennial screening mammograms at age 40. The specific frequency (1 or 2 years) is a decision to make with your provider based on personal risk.
· Cervical Cancer Screening: Continue with Pap/HPV testing.
· Blood Work: Increase vigilance with cholesterol, blood sugar (watch for pre-diabetes), and thyroid panels.
· Bone Density Scan: Not routine for all, but may be recommended if you have risk factors for osteoporosis (family history, steroid use, early menopause).
· Eye Health: Baseline screening for glaucoma and macular degeneration begins at 40.
· Heart Health: Cardiovascular risk increases. Discuss your numbers (blood pressure, cholesterol, weight) and any symptoms like fatigue or shortness of breath.
Your 50s & Beyond: Honoring Your Wisdom

This is about preserving quality of life, managing any chronic conditions, and celebrating longevity.
· Mammograms: Continue screening through at least age 74, in consultation with your doctor.
· Cervical Cancer Screening: Can often stop at age 65 if you have a adequate prior screening history and no high-risk history. Confirm with your provider.
· Colon Cancer Screening: Begin at age 45. Options include colonoscopy (every 10 years if normal), FIT stool test (annual), or others. This is a critical, life-saving screening.
· Bone Density Scan (DEXA): Recommended for all women at age 65, or earlier for those with risk factors.
· Lung Cancer Screening: An annual low-dose CT scan is recommended if you have a significant smoking history (talk to your doctor about criteria).
· Heart & Metabolic Health: Continued monitoring of blood pressure, cholesterol, and blood sugar. Discuss vaccines like Shingrix (shingles) and pneumococcal.
· Hearing Test: Baseline and then periodic checks.
· Mental & Cognitive Health: Keep your brain active and discuss any memory concerns with your provider.
The Most Important Item on the Checklist: You.
This roadmap is based on general guidelines for average-risk women. You are not average. Your personal and family health history, lifestyle, and ethnicity all shape your unique needs.
Your Action Items:

1. Bookmark this list as a conversation starter.
2. Schedule your annual wellness visit.
3. Come prepared with your family history, personal concerns, and this checklist.
4. Partner with your provider to create a personalized, proactive plan.
Preventative care is the ultimate act of self-respect. Here’s to knowing your body, advocating for your health, and thriving through every chapter.
FAQs
General Questions
Q: I feel healthy. Do I really need all these screenings?
A: Yes. Many serious conditions (like high blood pressure, high cholesterol, early-stage cancers, and prediabetes) are “silent” and show no symptoms until they’re advanced. Screenings are designed to catch these issues early when they are most treatable and manageable. Think of it as preventative maintenance—you change your car’s oil not because the engine has failed, but to prevent it from failing.

Q: How do I know if I’m “average risk” or “high risk”?
A: You are typically considered higher risk if you have:
· A first-degree relative (parent, sibling, child) with a history of cancers (especially breast, ovarian, colon) or heart disease at a young age.
· A known genetic mutation (e.g., BRCA, Lynch syndrome).
· A personal history of precancerous conditions (like atypical breast hyperplasia).
· Specific lifestyle or health factors (e.g., significant smoking history, diagnosis of HIV, a suppressed immune system).
The best course of action is to discuss your complete family and personal history with your provider at your next visit.
Q: What if I can’t afford all these screenings?
A: In many countries, preventative care screenings are covered at no cost under insurance plans. Check with your provider about coverage.
· Ask about costs upfront: Before any test, ask your doctor’s office and your insurance company about out-of-pocket costs.
· Look for resources: Community health centers, Planned Parenthood clinics, and local health departments often offer sliding-scale fees or free screenings for breast, cervical, and heart health.
· Prioritize: Your doctor can help you prioritize the most critical screenings based on your age and risk factors.
Decade-Specific Questions
In Your 20s & 30s
Q: I’m in my 20s. Do I need to think about breast cancer screening?
A: Formal mammograms aren’t routine until 40 for average-risk women. However, breast self-awareness (knowing what’s normal for you) and reporting any changes (a new lump, skin dimpling, nipple changes) to your doctor is crucial at any age. A clinical breast exam may be part of your annual visit.
Q: I’ve had the HPV vaccine. Do I still need Pap smears?
A: Yes, absolutely. The HPV vaccine protects against the most high-risk strains, but not all of them. Cervical cancer screening (Pap and/or HPV tests) remains essential according to the recommended schedule.
Q: When should I start thinking about fertility?
A: It’s never too early for a conversation. Even in your 20s, discussing your reproductive timeline with your provider is wise. In your 30s, if you think you might want children someday, a preconception counseling visit can address nutrition, supplements (like folic acid), chronic conditions, and overall health optimization.
In Your 40s & 50s+

Q: I’m terrified of getting a mammogram. Is it really that bad?
A: The discomfort is brief (a matter of seconds of compression) and the benefit is immense. Tips for an easier experience: schedule it for the week after your period when breasts are less tender, avoid caffeine for a few days prior, and take an over-the-counter pain reliever an hour before. Communicate with the technologist—they can work with you to minimize discomfort. Remember: a few moments of discomfort can be life-saving.
Q: I heard conflicting advice about when to start mammograms (40 vs. 50). Why?
A: Different expert groups weigh the benefits (early detection) and potential harms (false positives, anxiety, unnecessary biopsies) slightly differently. The prevailing trend, supported by organizations like the American College of Obstetricians and Gynecologists (ACOG), is to start at 40 for average-risk women. The key is to have a personalized discussion with your doctor about your risk tolerance and family history to decide on the best start time and frequency for you.
Q: Do I really need a colonoscopy at 45? What are the alternatives?
A: Colon cancer is highly preventable with screening. Starting at 45 is now the standard due to rising rates in younger adults.
· Colonoscopy: The “gold standard.” Done every 10 years if normal. It can both detect and remove precancerous polyps during the procedure.
· Alternatives: Stool-based tests like the FIT test (annual) or Cologuard (every 3 years) are non-invasive but are less accurate. If they come back positive, a colonoscopy is the necessary next step. Discuss the pros and cons of each option with your doctor.
Q: I’m over 65 and my periods have long stopped. Why am I still getting Pap smear reminders?
A: You can likely stop! Guidelines agree that women over 65 with adequate prior screening history (e.g., regular normal Pap/HPV tests for the past 10 years) and no history of high-grade precancerous changes can discontinue cervical cancer screening. Confirm this with your provider so they can officially update your chart.
Lifestyle & Follow-Up Questions

Q: How can I prepare for my annual wellness visit to make the most of it?
A: Be a prepared partner:
1. Write down any questions or concerns (changes in your body, sleep, mood, energy).
2. Know your family history (update it if a parent or sibling is newly diagnosed with something).
3. Bring a list of all medications and supplements you take.
4. Be honest about your lifestyle (diet, exercise, alcohol, stress, sexual health).
Q: What’s the single most important thing I can do for my health besides screenings?
A: Know your numbers and live a heart-healthy lifestyle. This forms the foundation. Know your blood pressure, cholesterol, blood sugar, and BMI. The lifestyle choices that protect your heart—a balanced diet, regular movement, not smoking, managing stress, and quality sleep—also dramatically lower your risk for numerous cancers, diabetes, and cognitive decline.
Q: What happens if a screening test comes back “abnormal”?
A: First, don’t panic. An abnormal result is not a diagnosis. It is a signal that needs further investigation. It could be a false positive, a benign (non-cancerous) finding, or a very early-stage issue. Your provider will guide you on the next steps, which may include a repeat test, a more detailed imaging test (like an ultrasound), or a biopsy. The entire point of screening is to find these things at a stage where they are highly manageable.