For years, cholesterol has been cast as a villain in the story of heart health. But this narrative is incomplete and misleading. The truth is, cholesterol isn’t inherently “bad”—it’s a vital, waxy substance your body uses to build cells and make hormones. The real story is about transportation, not just the passenger. Understanding the difference between LDL and HDL, and what your ratios truly mean, is the key to taking control of your cardiovascular health.

Meet the Carriers: LDL and HDL Explained
Think of your bloodstream as a waterway. Cholesterol, being fatty, can’t dissolve in blood (like oil in water). It needs to be carried by special proteins called lipoproteins. This is where the “good” and “bad” labels come from, based on what these lipoproteins do.
LDL (Low-Density Lipoprotein): The “Potential” Problem
· The Label: “Bad” Cholesterol.
· The Job: LDL is a delivery truck. It carries cholesterol from your liver (where it’s made) out to the parts of your body that need it.
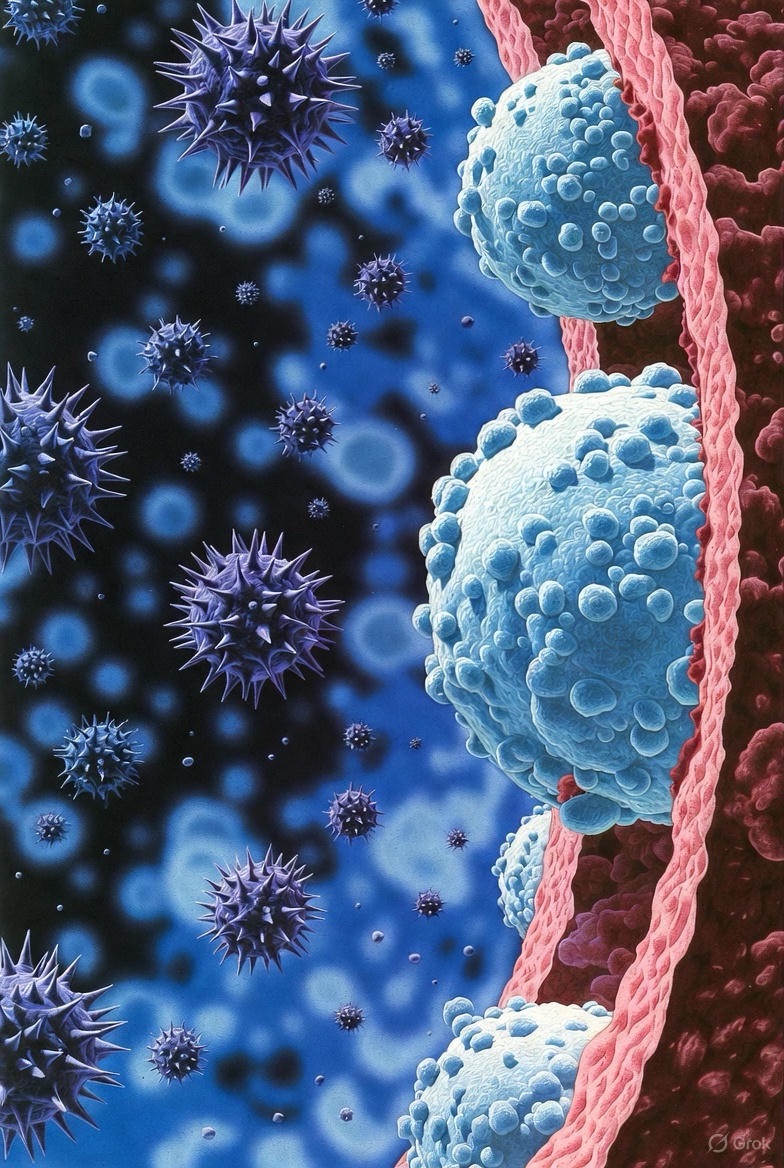
· Why It Gets a Bad Rap: When there’s too much LDL in the blood, it can start to deposit cholesterol into the walls of your arteries. This forms a sticky, thick substance called plaque—a process called atherosclerosis. Plaque narrows arteries, making them stiff and less flexible. If a plaque ruptures, it can cause a clot that blocks blood flow, leading to a heart attack or stroke.
Key Takeaway: LDL isn’t evil, but high levels are a major risk factor for cardiovascular disease. Modern science also looks at the size and type of LDL particles—small, dense particles are more dangerous than large, fluffy ones.
HDL (High-Density Lipoprotein): The Cleanup Crew
· The Label: “Good” Cholesterol.
· The Job: HDL is a garbage truck. It travels through your bloodstream, picks up excess cholesterol from your arteries and tissues, and transports it back to your liver for disposal or recycling.
· The Benefit: This process is called reverse cholesterol transport, and it helps keep your arteries clear. Higher levels of HDL are generally associated with a lower risk of heart disease.
Key Takeaway: Think of HDL as your arterial maintenance team. You want a strong, efficient crew.
The Magic Number Isn’t Just a Number: Understanding Your Ratios
While individual LDL and HDL numbers matter, cardiologists now emphasize that the relationship between them is often more telling for your heart risk than any single figure.
Here are the two most critical ratios:
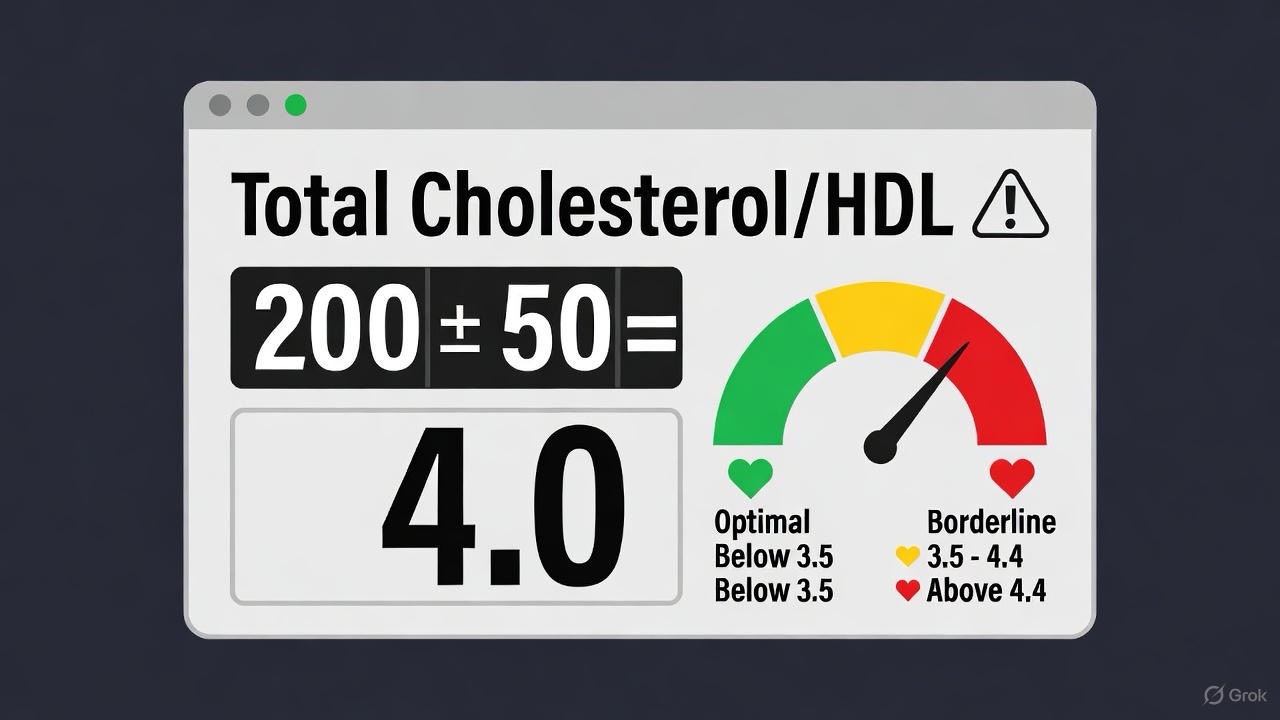
1. Total Cholesterol to HDL Ratio
· Formula: (Total Cholesterol) / (HDL)
· What it means: This is considered one of the best predictors of heart disease risk. It tells you how much of your total cholesterol is “good” (HDL).
· Ideal: Below 3.5:1. A lower ratio is better.
· Example: If your Total Cholesterol is 200 mg/dL and your HDL is 50 mg/dL, your ratio is 4:1 (200/50). If you raise your HDL to 60 mg/dL, your ratio improves to 3.3:1.
2. LDL to HDL Ratio
· Formula: (LDL) / (HDL)
· What it means: This directly compares your primary risk factor (LDL) to your primary protector (HDL).
· Ideal: Below 2:1. Again, lower is better.
· Example: An LDL of 120 mg/dL and an HDL of 40 mg/dL gives a high-risk ratio of 3:1. Improving your diet and exercise to change those numbers to LDL 100 and HDL 50 gives a healthier 2:1 ratio.
Why Ratios Matter More
A person with a “high” total cholesterol of 240 might be at low risk if their HDL is a robust 80 (ratio: 3:1). Conversely, someone with a “normal” total cholesterol of 180 could be at higher risk if their HDL is only 30 (ratio: 6:1). Ratios provide crucial context.
What Your Action Plan Should Look Like
You have significant power to influence your cholesterol numbers and ratios through lifestyle.
To Lower LDL (“Bad”):
· Reduce Saturated & Trans Fats: Limit red meat, full-fat dairy, fried foods, and processed baked goods.
· Increase Soluble Fiber: Oats, beans, lentils, apples, and psyllium husk can bind to cholesterol and help remove it.
· Incorporate Healthy Fats: Avocados, olive oil, nuts, and fatty fish (like salmon) support healthier lipid profiles.
· Move Regularly: Aim for at least 150 minutes of moderate aerobic exercise per week.
To Raise HDL (“Good”):
· Cardio is Key: Aerobic exercise is one of the most effective ways to boost HDL.
· Choose Healthy Fats: Monounsaturated and polyunsaturated fats support HDL levels.
· Don’t Smoke: Quitting smoking can raise HDL significantly.
· Maintain a Healthy Weight: Losing excess weight can help increase HDL.

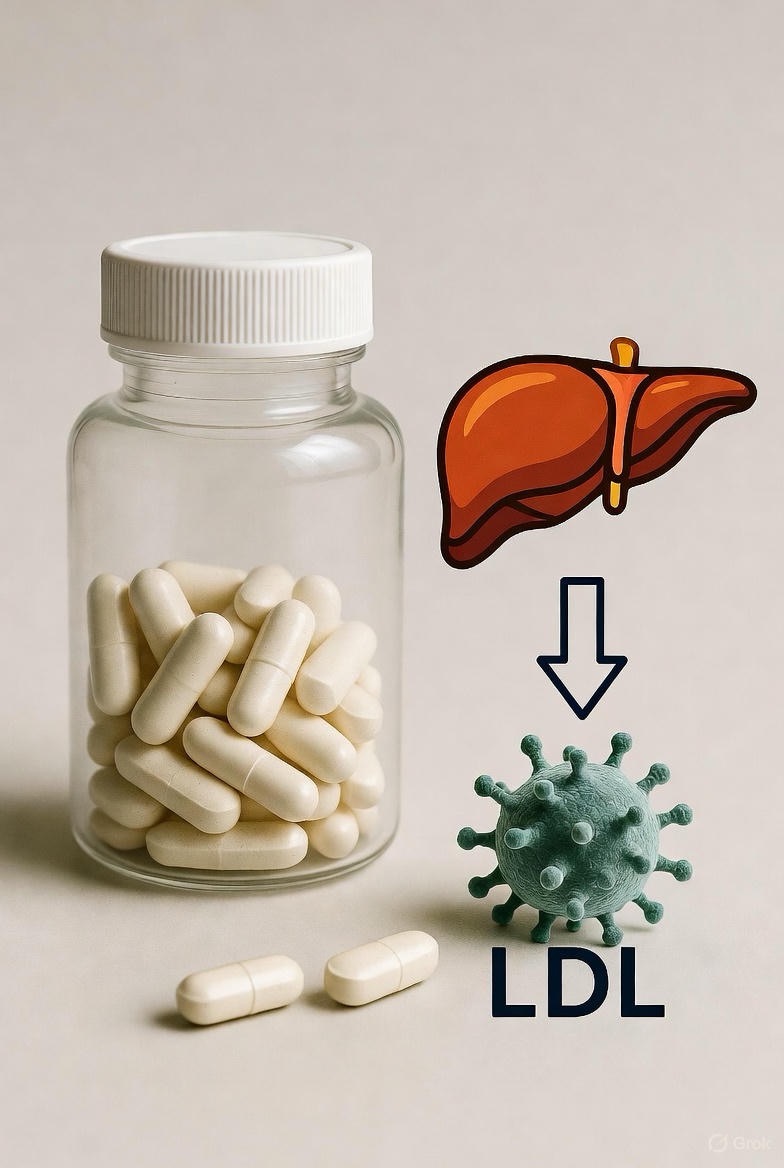
When Lifestyle Isn’t Enough: The Role of Medication
For some, genetics play a dominant role (a condition called familial hypercholesterolemia). No amount of oatmeal can fully counteract it. In these cases, statins and other medications are life-saving tools. They work primarily in the liver to dramatically reduce LDL production and have proven, unequivocal benefits in preventing heart attacks and strokes.
The Bottom Line
Stop viewing cholesterol as a simple “good vs. bad” battle. Instead, see it as a complex transportation system that needs balance. Your goal is to minimize the LDL delivery trucks getting stuck in your arterial streets and maximize the HDL cleanup crews.
Your Next Step: Get a full lipid panel at your next physical. Don’t just look at the total number. Examine your LDL, HDL, and—most importantly—your ratios. Have a conversation with your doctor about what these numbers mean for you, in the context of your overall health, family history, and other risk factors. Empowered with this knowledge, you can build a targeted plan for a healthier heart.
FAQs
1. If my total cholesterol is high, but my HDL is also high, should I worry?
Answer: Not necessarily. This is exactly why ratios matter more than the total number. A high total cholesterol driven by a very high HDL (the “good” garbage truck) is often protective. Calculate your Total Cholesterol/HDL ratio. If it’s below 3.5:1, your risk may be lower than someone with a “normal” total cholesterol but low HDL. Always discuss the full breakdown with your doctor.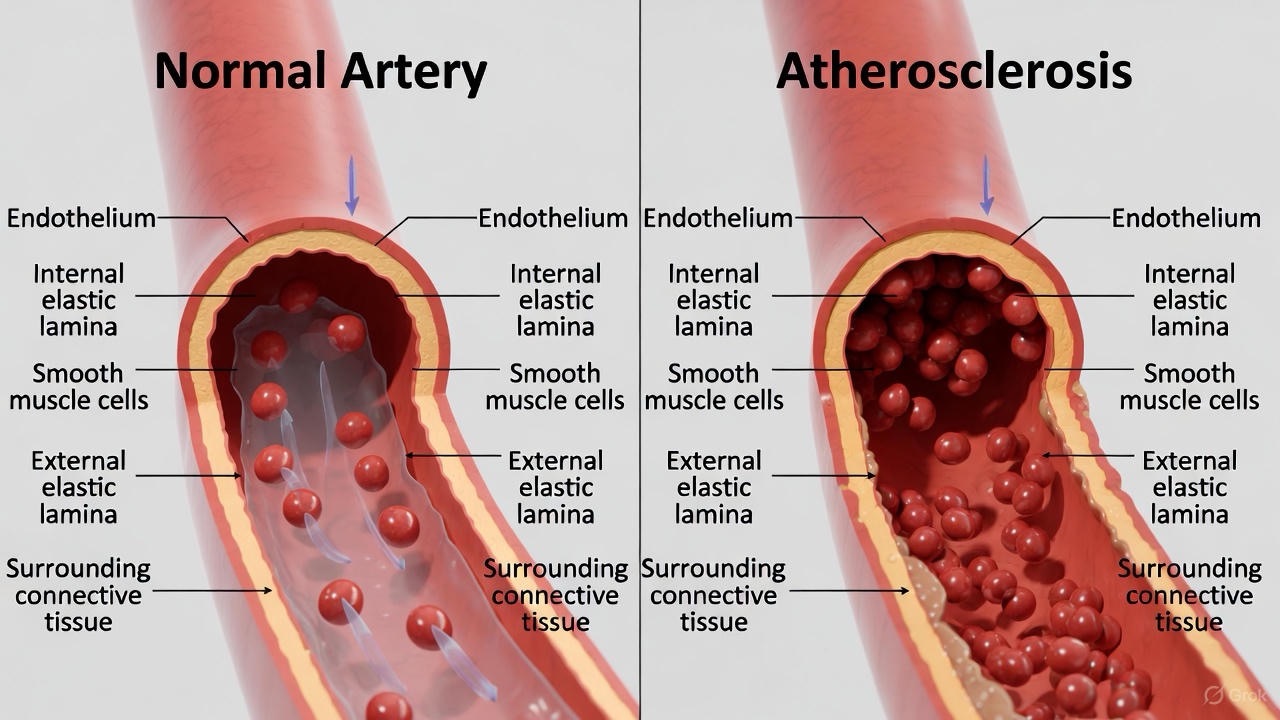
2. Can I have high cholesterol even if I’m young, fit, and eat well?
Answer: Yes, absolutely. This is often due to genetics, specifically a condition called familial hypercholesterolemia (FH). FH causes the liver to be inefficient at removing LDL from the blood, leading to very high LDL levels from a young age, regardless of lifestyle. If you have a family history of early heart disease (e.g., in parents or siblings under 55/65), ask your doctor about screening for FH.

3. Are eggs really bad for my cholesterol?
Answer: For most people, no. Dietary cholesterol (from eggs, shellfish) has a much smaller impact on blood cholesterol than previously thought. The bigger culprits are saturated and trans fats (found in processed foods, fried items, fatty cuts of meat). Eggs are a nutrient-dense source of protein. Current guidelines suggest that for healthy individuals, consuming 7-12 eggs per week is generally fine and does not significantly raise heart disease risk.
4. What’s the difference between LDL and “bad cholesterol”?
Answer: “Bad cholesterol” is a simplified label for LDL-cholesterol. LDL itself is the low-density lipoprotein (the delivery truck). The cholesterol it carries is the cargo. When we say “your LDL is 130,” we’re measuring the amount of cholesterol cargo inside the LDL trucks. High levels mean too many trucks are delivering cargo that can get stuck in your artery walls.
5. Is there such a thing as “good” LDL or “bad” HDL?
Answer: This gets into advanced particle science.
· LDL Particles: Yes, there are different types. Small, dense LDL particles are more dangerous—they can easily penetrate artery walls and oxidize. Large, fluffy LDL particles are considered less risky. Standard blood tests don’t always show this; you may need an advanced lipid panel.
· HDL Function: Emerging research shows that HDL function (how well it cleans up cholesterol) may be more important than just the amount. In some inflammatory diseases (like severe rheumatoid arthritis), HDL can become dysfunctional (“bad”) and actually contribute to plaque. This is an active area of research.
6. My doctor wants me on a statin, but my cholesterol isn’t “that high.” Why?
Answer: Cholesterol treatment decisions are based on overall cardiovascular risk, not just a number. Your doctor uses calculators that consider your age, blood pressure, smoking status, diabetes, AND cholesterol to estimate your 10-year risk of a heart attack or stroke. If that overall risk is high, a statin is recommended as a preventative measure, even with moderately elevated LDL, because statins reduce inflammation and stabilize plaque beyond just lowering LDL.
7. What are triglycerides, and how do they fit in?
Answer: Triglycerides are the most common type of fat in your body, storing excess energy from your diet. High triglycerides are an independent risk factor for heart disease and often accompany low HDL, high LDL, and insulin resistance (a pattern called “atherogenic dyslipidemia”). They are highly influenced by diet—especially excess sugar, refined carbs, and alcohol.
8. Can I improve my cholesterol with diet alone?
Answer: For many people, yes, significantly. The portfolio diet approach—which combines multiple cholesterol-lowering foods—has been shown to reduce LDL as effectively as some low-dose statins. This includes:
· Soluble fiber (oats, barley, beans, psyllium).
· Plant sterols/stanols (found in some fortified foods).
· Nuts (a handful of almonds or walnuts daily).
· Soy protein (tofu, tempeh).
· Healthy fats (avocado, olive oil).
However, for those with genetic conditions like FH, medication is usually necessary alongside diet.
9. Why is my HDL low, and how can I raise it?
Answer: Common causes of low HDL include:
· Sedentary lifestyle
· A diet high in refined carbs and sugar
· Smoking
· Excess body weight, particularly around the waist
· High triglycerides
To raise HDL, focus on: Aerobic exercise (most effective), quitting smoking, replacing refined carbs with healthy fats (avocado, nuts, olive oil), and losing excess weight.
10. What’s a better predictor of heart risk: LDL number or the LDL/HDL ratio?
Answer: In current cardiology practice, both are critically important, but they are used for different things.
· LDL-C (the number): This is the primary treatment target. Guidelines set specific LDL goals based on your risk category (e.g., below 100 mg/dL for moderate risk, below 70 mg/dL for high risk).
· Ratios (Total/HDL, LDL/HDL): These are excellent risk assessment tools. They provide a snapshot of your overall lipid balance and are powerful predictors of future events. A high LDL with a terrible ratio is a red flag. Your doctor will use both.

11. Should I get an advanced lipid panel?
Answer: Consider it if you have:
· A personal or strong family history of early heart disease.
· High cholesterol that doesn’t respond well to treatment.
· High triglycerides or metabolic syndrome.
An advanced panel measures LDL particle number (LDL-P) and size, which can sometimes reveal high risk even when standard LDL-C looks “normal.” Discuss with your doctor if it’s right for you.
12. How often should I get my cholesterol checked?
Answer:
· Adults 20+: Get a baseline test at least once every 4-6 years if risk is low.
· If you have risk factors (high BP, diabetes, smoking, family history, overweight): Get tested more frequently, often annually.
· If you are on cholesterol-lowering medication: You will be tested regularly (e.g., every 3-12 months) to monitor effectiveness and safety.

