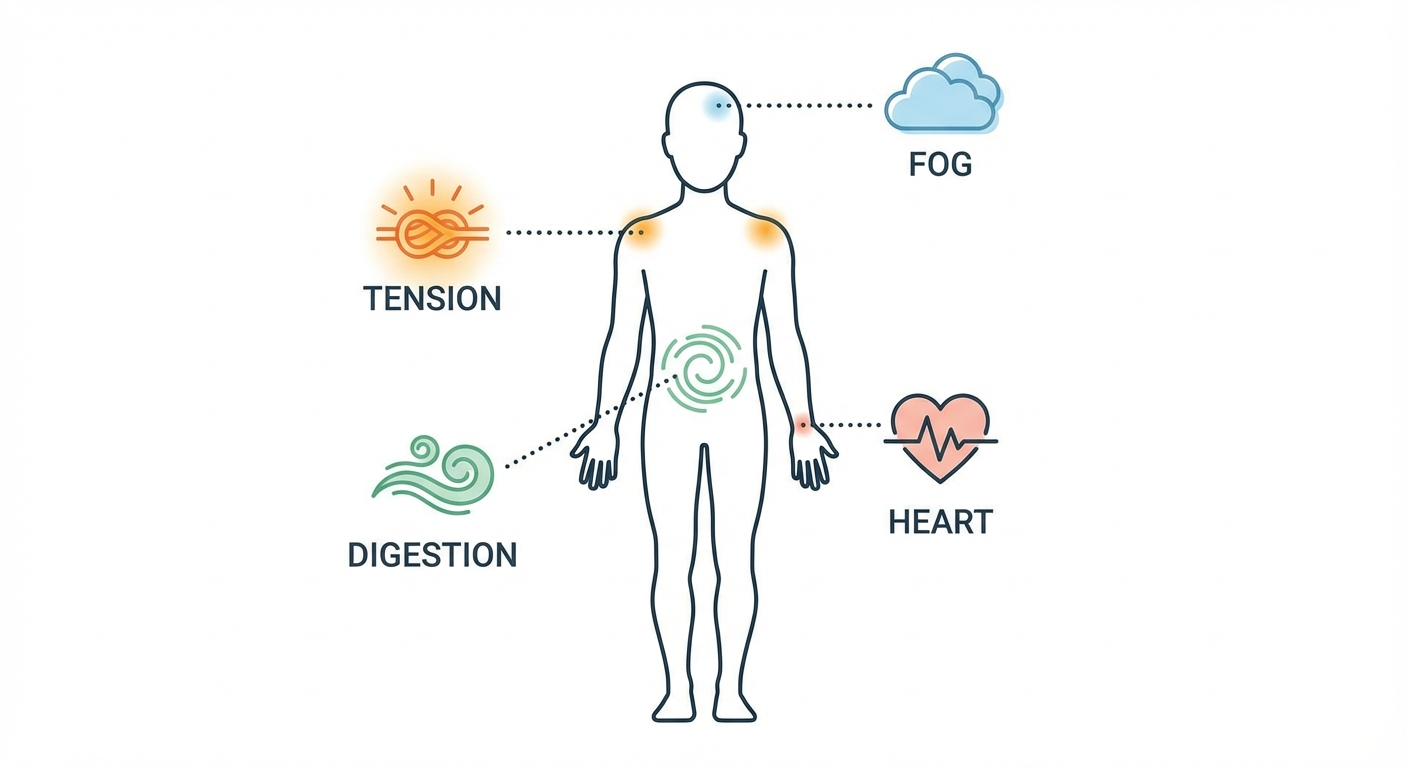
We often think of anxiety as a condition of the mind—racing thoughts, persistent worry, a sense of impending doom. But anxiety doesn’t just live in your head; it speaks through your body. In fact, for many people, the first red flag isn’t a feeling of nervousness at all, but a mysterious, recurring ache or ailment.
If you’ve been chasing physical symptoms with no clear medical cause, you might be experiencing what experts call somatic anxiety—the body’s tangible expression of psychological distress. Recognizing these signs is the first step toward finding real relief.

Your Gut: The “Second Brain”
One of the most common arenas for anxiety is your digestive system, often called the enteric nervous system or the “second brain.”
What you might feel:
· Unexplained IBS-like symptoms: Bloating, cramps, and alternating diarrhea or constipation without a clear dietary trigger.
· Chronic nausea or “butterflies”: A persistent, unsettled feeling in your stomach, especially before events or decisions.
· Loss of appetite or nervous hunger: Anxiety can flip your hunger signals completely off or into overdrive.
The Science: The brain and gut are in constant communication via the vagus nerve. When your brain sounds the alarm (anxiety), your gut listens, diverting energy from digestion as part of the “fight-or-flight” response, leading to discomfort and dysfunction.
The Unrelenting Grip: Muscle Pain and Tension
Do you often feel like you’ve been through a workout, but you haven’t? Chronic, unexplained muscle pain is a hallmark of somatic anxiety.

What you might feel:
· A tight jaw or TMJ pain, especially upon waking (from clenching at night).
· A persistent stiff neck and shoulders, often described as “carrying the weight of the world.”
· Generalized aches, particularly in the back, as if you can’t ever get comfortable.
The Science: Under stress, your muscles unconsciously contract to prepare for perceived danger. Chronic anxiety means they never get the signal to fully relax, leading to pain, tension headaches, and fatigue.

The Relentless Throb: Headaches and Fatigue
Not all headaches are from dehydration or eye strain. Anxiety can fuel a specific type of pain.
What you might feel:
· Tension headaches: A constant, dull band of pressure around your forehead or at the base of your skull.
· “Brain fog” and exhaustion: A profound fatigue that sleep doesn’t fix, accompanied by a sense of mental murkiness.
· Dizziness or lightheadedness, a feeling of being slightly ungrounded or off-balance.
The Science: Chronic anxiety floods your system with stress hormones like cortisol. This can disrupt sleep architecture (even if you’re logging hours), prevent deep restorative rest, and cause sustained muscle tension that manifests as headache pain.
The Lesser-Known Signals
Anxiety’s physical vocabulary is vast. Other often-missed symptoms include:
· Skin flare-ups: Stress can exacerbate eczema, psoriasis, or hives.
· Hair loss (Telogen Effluvium): Significant stress can shock hair follicles into a resting phase, leading to increased shedding months later.
· Tinnitus or ear ringing: Heightened nervous system activity can amplify your perception of internal sounds.
· Frequent illness: Chronic stress and anxiety can suppress your immune system, making you more susceptible to colds and infections.
What To Do If Your Body Is Sending Signals
1. Rule Out the Purely Physical First. Always consult a doctor (like a GP or internist) to investigate these symptoms. This is a crucial step to rule out other conditions and validate your experience.
2. Connect the Dots. Start a simple journal. Note your physical symptom (e.g., “3 PM, migraine started”) and any preceding emotions or stressors (e.g., “overwhelmed with inbox, meeting at 2 PM”). Patterns will emerge.
3. Treat the Body to Soothe the Mind. You can start here, even while seeking answers:
· Progressive Muscle Relaxation: Systematically tense and release muscle groups.
· Deep Belly Breathing: Activates the parasympathetic (“rest and digest”) nervous system.
· Gentle Movement: Walking, yoga, or stretching can release pent-up muscular tension.
4. Seek Professional Mental Health Support. If a medical workup comes back clear, consider speaking with a therapist. Cognitive Behavioral Therapy (CBT) is particularly effective for somatic symptoms, as it helps reframe the thought patterns that trigger the physical response. A psychiatrist can also discuss if medication might help break the cycle.
You Are Not Making It Up
If you take away one thing, let it be this: These physical symptoms are real. They are not “all in your head” in the dismissive sense. They are the very real, biological output of a nervous system that’s working overtime to protect you.
Listening to your body’s hidden language of anxiety isn’t about pathologizing every ache. It’s about becoming a compassionate detective of your own well-being. By addressing the root anxiety, you often find that the mysterious physical symptoms begin to lose their power, allowing you to find a path to greater peace—both in mind and body.
If you see yourself in these signs, know that help and understanding are available. Your body is trying to tell you something. It’s time we learn to listen.

FAQs
Q1: How can I tell if my stomach issues are from anxiety or a physical condition like IBS or a food intolerance?
A: This is a crucial distinction. Anxiety-induced gut issues often correlate directly with stress levels—flaring up before big meetings, during conflict, or in periods of overwhelm. A key clue is if medical tests (like for celiac disease, infections, or intolerances) come back normal. True IBS can also be severely exacerbated by anxiety, creating a cycle. The best path is to see a gastroenterologist to rule out primary physical causes first, then work with a therapist if anxiety appears to be a major trigger or contributor.

Q2: Can anxiety cause pain in places I’ve been injured before, like an old back injury?
A: Absolutely. Anxiety increases overall inflammation and muscle tension in the body. An old injury site is often a “weak link” in your system—a place where tension and pain manifest most easily. Your nervous system may also become hypersensitive in that area. It’s not that the pain isn’t real; it’s that the anxiety is amplifying the pain signal from that previously vulnerable spot.
Q3: I don’t feel mentally “anxious,” so how can my headaches/eczema/fatigue be caused by anxiety?
A: This is a very common experience. Anxiety isn’t always conscious worry. It can operate as a background process in your nervous system—a state of chronic, low-grade hyperarousal that you’ve adapted to. Your body can be in a stress response (releasing cortisol, tensing muscles) due to subconscious worries, past trauma, or chronic life pressures, even if your conscious mind feels numb or “fine.” The body often keeps the score.
Q4: Are panic attacks the same as these physical symptoms?
A: Panic attacks are an acute, intense peak of these physical symptoms. They involve a sudden, overwhelming surge where multiple symptoms (heart palpitations, shortness of breath, dizziness, chest pain, terror) hit at once. The symptoms described in the article are often the chronic, low-grade version—a constant hum of physical distress rather than a sudden siren. One can exist without the other.
Q5: Will treating my anxiety make my physical symptoms go away completely?
A: For many, yes—significantly or entirely. When the nervous system calms down, the physical output (muscle tension, gut irritation, inflammatory response) often subsides. For others, especially with co-existing conditions (like true IBS or chronic migraines), anxiety management becomes a powerful tool to reduce the frequency and severity of flares. It’s a central part of the treatment plan.

Q6: What kind of doctor should I see for this? I feel shuffled between specialists.
A: Start with your Primary Care Physician (PCP). Be explicit: “I’m experiencing these physical symptoms, and I wonder if anxiety could be a contributing factor. Can we rule out other causes?” Your PCP can run baseline tests and then refer you appropriately—to a gastroenterologist, dermatologist, etc., for specific symptoms and/or to a therapist or psychiatrist. An integrated approach is best.
Q7: Can anxiety medication help with physical symptoms?
A: Often, yes. SSRIs (a common class of antidepressants used for anxiety) can help regulate the nervous system’s overactivity, which in turn can reduce muscle tension, gut sensitivity, and inflammatory responses. They are not just “happy pills”; they work on the biological pathways that translate mental distress into physical symptoms. This is a discussion for a psychiatrist.
Q8: Are there any immediate physical techniques to stop a symptom flare-up?
A: Yes. Try “belly breathing” or “box breathing” to activate your vagus nerve and parasympathetic (calming) system. For muscle clenching, try progressive muscle relaxation: tense a muscle group (clench fists) tightly for 5 seconds, then release fully for 30 seconds, moving through the body. For acute gut distress, a heating pad on the abdomen can soothe cramping muscles.

Q9: Is it dangerous to ignore these physical symptoms?
A: While the symptoms themselves are typically not life-threatening, chronic untreated stress and anxiety are major risk factors for long-term health issues like hypertension, heart disease, and autoimmune disorders. Furthermore, ignoring them prolongs suffering and decreases your quality of life. Addressing the root cause is an act of preventive healthcare.
Q10: How do I explain to my doctor that I think it’s anxiety without feeling dismissed?
A: Use a factual, symptom-led approach. Instead of leading with “I think this is anxiety,” try: “I have chronic headaches (or stomach pain). My research shows anxiety can be a cause. We’ve ruled out X, Y, and Z. Can we explore the mind-body connection here? Would a referral to a therapist be appropriate as part of my treatment plan?” This frames it as a collaborative investigation.

Q11: Can children have physical symptoms of anxiety?
A: Yes, and frequently. Children often lack the vocabulary to express emotional worry, so it comes out physically. Common signs are frequent stomachaches, headaches, refusal to go to school, restlessness, and changes in sleep patterns. It’s vital to take these complaints seriously and seek evaluation from a pediatrician and potentially a child psychologist.
Q12: If I start therapy for anxiety, how long before I see physical improvement?
A: It varies, but some people notice a subtle shift in 3-4 weeks as they learn to interrupt the stress response. More significant physical relief often comes with sustained practice over 2-3 months. Think of it as retraining a well-worn pathway in your nervous system—it takes consistent repetition to build a new, calmer default setting.

