Pressure ulcers—also known as bedsores or pressure injuries—are more than just skin deep. They represent a significant challenge for individuals with limited mobility and those who care for them. These painful wounds develop when sustained pressure cuts off blood flow to vulnerable areas of the body, leading to tissue damage. For caregivers and patients alike, understanding how to prevent and manage pressure ulcers is a critical component of maintaining health, dignity, and quality of life.
This guide will walk you through the essential knowledge and practical steps needed to protect skin integrity and promote healing.
What Are Pressure Ulcers?
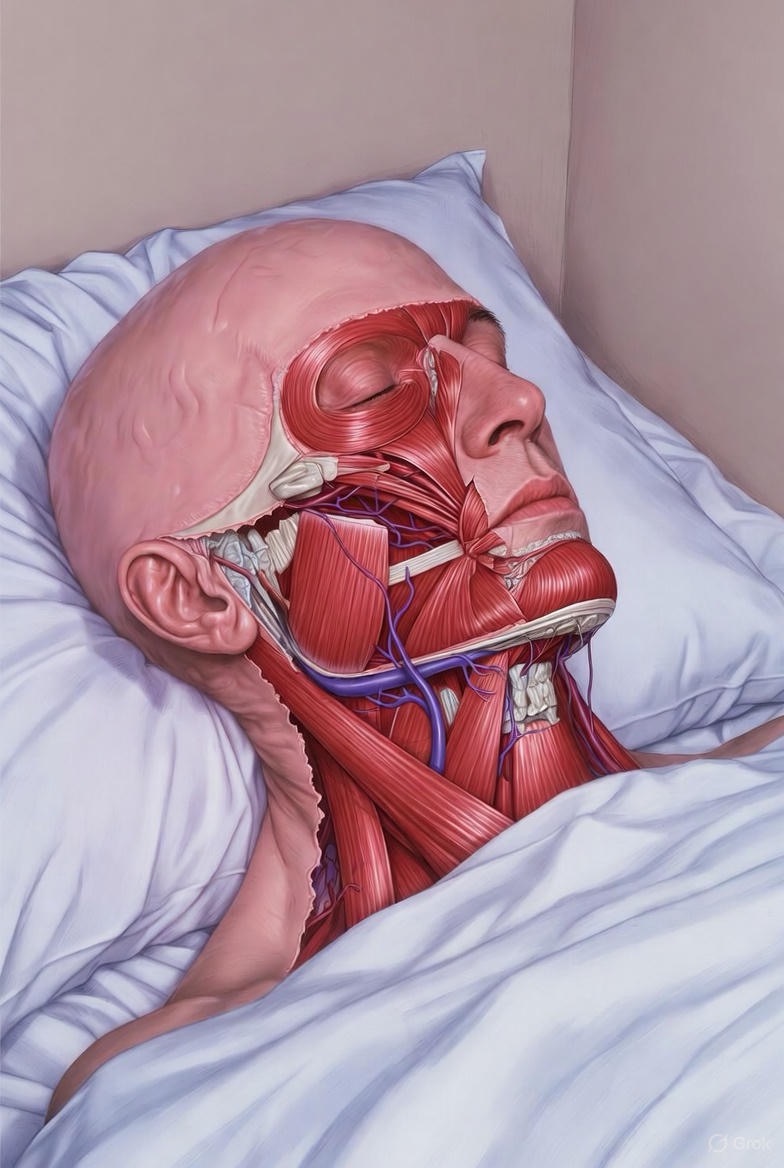
Pressure ulcers are localized injuries to the skin and underlying tissue, typically over a bony prominence, caused by intense or prolonged pressure combined with shear (sliding) or friction. They most commonly occur on the:
· Heels and ankles
· Tailbone (sacrum) and buttocks
· Hips
· Spine and shoulder blades
· Backs of the head and ears
They are staged from 1 to 4 based on their severity, with Stage 1 being the earliest sign (persistent redness) and Stage 4 involving full-thickness tissue loss with exposed bone, muscle, or tendon.
The High Cost of Pressure Ulcers
Beyond the physical pain, pressure ulcers can lead to serious complications like bone and joint infections, cellulitis, and even sepsis. They drastically reduce quality of life, prolong hospital stays, and increase healthcare costs. The most important fact to remember is this: Most pressure ulcers are preventable with consistent, attentive care.
The Pillars of Prevention: A Caregiver’s Action Plan
Prevention is always the best medicine. A proactive, multi-faceted approach is key.
1. Relieve Pressure Through Repositioning
· The Two-Hour Rule: Reposition a bed-bound person at least every two hours. Use a schedule (e.g., left side, back, right side).
· For Chair Users: Shift weight every 15 minutes. If possible, assist them to stand or reposition hourly.
· Use Proper Positioning Aids: Pillows, foam wedges, and specialized heel protectors can keep bony areas from direct contact.
· Invest in Support Surfaces: Consider a pressure-redistributing alternating pressure mattress or medical-grade foam overlay. For wheelchairs, use a pressure-relieving cushion.

2. Conduct Daily Skin Inspections
Make this a non-negotiable part of the daily routine. Check all at-risk areas in good light. Look for:
· Persistent redness that doesn’t fade when pressure is removed (the first sign of a Stage 1 ulcer)
· Changes in skin temperature (warmth or coolness), texture (hardness or boggy feel), or color (purple/blue hues in darker skin)
· Blisters, open sores, or scabs
Tip: Use a mirror for hard-to-see areas or ask for help. Document any changes.
3. Practice Meticulous Skin Care
· Keep Skin Clean and Dry: Cleanse gently with a pH-balanced, mild soap and lukewarm water. Pat—don’t rub—skin dry.
· Manage Moisture: Incontinence, sweat, or wound drainage can macerate skin. Use moisture-barrier creams or ointments (like zinc oxide). Consider absorbent pads or breathable incontinence products.
· Protect from Shear and Friction: Use proper lifting techniques (never drag across sheets). Use satin or low-friction sheets and pajamas. Ensure the head of the bed is raised no more than 30 degrees when possible to prevent sliding.
4. Support Nutrition and Hydration
Malnutrition and dehydration are major risk factors.
· Ensure Adequate Protein: Protein is essential for tissue repair. Include lean meats, eggs, dairy, beans, and supplements if recommended.
· Promote Vitamin & Mineral Intake: Vitamins A, C, and zinc are crucial for skin health. Serve plenty of fruits and vegetables.
· Encourage Fluid Intake: Aim for proper hydration unless medically restricted. Offer water frequently.
A Step-by-Step Guide to Care for an Existing Pressure Ulcer
If a pressure ulcer develops, immediate and careful action is required. Always consult with a healthcare professional (doctor or wound care nurse) for a treatment plan.
Step 1: Seek Professional Assessment
A healthcare provider will determine the stage, size, and presence of infection. They will develop a tailored treatment plan, which may include debridement (removal of dead tissue), specialized dressings, and managing infection.
Step 2: Relieve ALL Pressure
The wound must be completely offloaded. This is non-negotiable. Use positioning devices to create a “bridge” so the ulcerated area has no contact with any surface.
Step 3: Provide Meticulous Wound Care
· Cleanse Gently: Use a sterile saline solution or wound cleanser with each dressing change.
· Apply Appropriate Dressings: Modern dressings maintain a moist healing environment and protect the wound. Common types include:
· Hydrocolloids: For early-stage ulcers with minimal drainage.
· Foam Dressings: For moderate drainage.
· Alginate or Hydrofiber: For wounds with heavy drainage.
· Antimicrobial Dressings: If infection is a concern.
· Change Dressings as Directed: Follow the schedule set by your healthcare provider.

Step 4: Monitor for Signs of Infection
Watch for and report immediately:
· Increased pain, redness, swelling, or warmth around the wound
· Foul odor or pus (green/yellow drainage)
· Fever or chills
· The wound appears to be getting larger or deeper
The Emotional Toll: Caring for the Caregiver
Caring for someone at risk of pressure ulcers is demanding. Caregiver burnout is real. Remember:
· You are not alone. Seek support from family, friends, or support groups.
· Ask for help. Reach out to home health agencies for respite care or nursing assistance.
· Celebrate small victories. Successful prevention is a major achievement.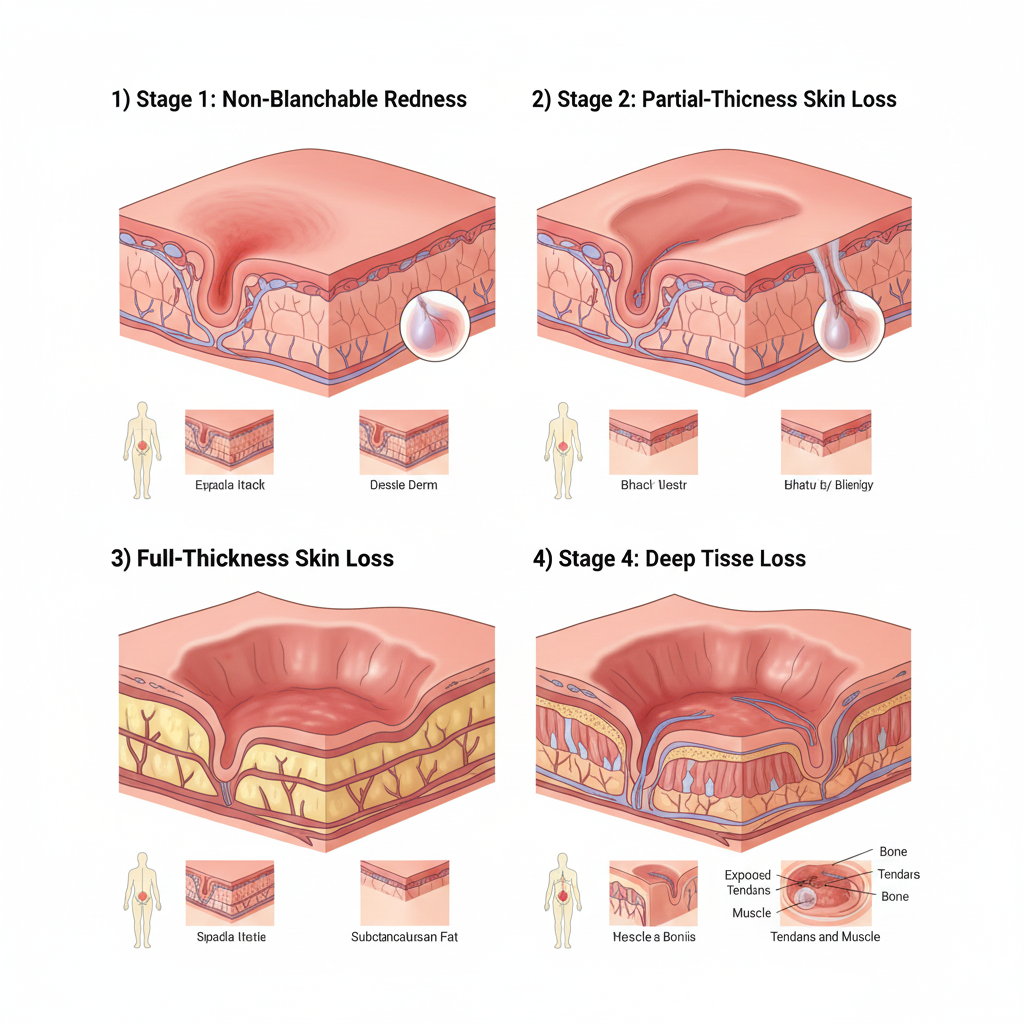
Final Message of Hope
Pressure ulcer prevention is a daily commitment that requires vigilance, knowledge, and compassion. By integrating these practices into a routine, caregivers become powerful agents of healing and comfort. For patients, understanding your own skin and speaking up about any discomfort empowers you to be an active partner in your care.
Your skin is your body’s largest organ. Protecting it is a profound act of care.
FAQs
1. How often should I reposition someone in bed to prevent bedsores?
Answer: For individuals at risk, repositioning should occur at least every 2 hours when in bed. For those in a chair or wheelchair, assist with a weight shift every 15-30 minutes, and a full reposition every hour. Always use a written schedule and check the skin after each move.
2. What’s the most important piece of equipment for prevention?
Answer: A high-quality pressure-redistributing support surface is critical. This can be an alternating pressure air mattress, a medical-grade foam overlay, or a specialized wheelchair cushion. It is not a replacement for turning, but it significantly reduces pressure points.

3. I see a red spot that doesn’t go away. Is that a pressure ulcer?
Answer: A persistent area of redness (or purple/darkened skin on darker complexions) that does not fade within 15-30 minutes after pressure is removed is a Stage 1 pressure ulcer. It’s a warning sign. You must ensure this area is completely off-loaded from pressure and monitored closely.
4. Can I use massage or rubbing alcohol on red areas?
Answer: No, absolutely not.
· Do not massage reddened bony areas, as this can cause further damage to tissue beneath the skin.
· Do not use rubbing alcohol or talcum powder, as they can dry and crack the skin. Use gentle cleansers, pat the area dry, and apply a moisture barrier cream if needed.
5. What’s the single best thing I can do for an existing pressure ulcer?
Answer: Get all pressure off the wound. This is the most critical step. You must use pillows, foam wedges, or specialized devices to “float” the area so it does not touch the bed or chair at all. Healing cannot begin if pressure continues.
6. What should a healthy pressure ulcer dressing look like?
Answer: A healthy wound bed under a modern dressing should be moist (not wet or dry) and show signs of healing like shrinking size and pink/red tissue (granulation tissue). Drainage should be minimal and clear or pale yellow. Report any increase in foul-smelling, green, or thick drainage immediately.
7. How does nutrition affect pressure ulcers?
Answer: Nutrition is fundamental. Protein is the building block for new tissue. Without adequate protein, vitamins (especially A, C, and E), zinc, and hydration, the body cannot repair skin. A dietitian can help create a plan, and supplements like protein shakes are often recommended.

8. Are there areas we commonly miss during skin checks?
Answer: Yes. Caregivers often miss:
· The backs of the heels and ankles
· The skin behind the knees
· The ears and back of the head
· Between skin folds (under breasts, abdomen, or groin)
Use a hand mirror and good lighting to check every bony prominence and skin fold daily.
9. My loved one is incontinent. How do I protect their skin?
Answer:
1. Clean gently and promptly after each episode with a no-rinse pH-balanced cleanser.
2. Pat dry thoroughly—never rub.
3. Apply a thick moisture barrier ointment or cream (like zinc oxide or dimethicone-based products) to create a protective layer.
4. Use highly absorbent, breathable incontinence products and change them frequently.

10. When is a pressure ulcer a medical emergency?
Answer: Seek immediate medical attention if you see:
· Signs of infection: Fever, chills, confusion, or foul-smelling pus.
· Systemic infection: Red streaks leading from the wound.
· Rapid worsening: The wound suddenly becomes much larger, deeper, or black (eschar).
· Sepsis symptoms: Fast heart rate, difficulty breathing, extreme pain.
11. Can someone with a pressure ulcer take a bath or shower?
Answer: Generally, yes, but with precautions:
· Showers are preferred over baths to minimize soaking.
· Protect the wound with a waterproof dressing if possible.
· Use lukewarm (not hot) water and mild soap, avoiding direct, harsh streams on the wound.
· Pat the area dry gently after, and reapply a clean, appropriate dressing.
12. What is “shear” and why is it as bad as pressure?
Answer: Shear is a mechanical force that occurs when skin sticks to a surface (like sheets) while the body slides down (e.g., when the head of the bed is raised). This stretches and tears blood vessels and tissues under the skin, causing deep damage that may not be visible on the surface. Prevent it by using proper lifting techniques (never drag), and keeping the head of the bed at or below a 30-degree angle when possible.
13. Is it ever okay to use a donut-shaped cushion?
Answer: No. Ring or donut-shaped cushions actually reduce blood flow to the area in the center (the wound) and can cause more harm. Use solid, pressure-redistributing cushions or foam pads designed to “float” the area.

14. How can I manage the pain of a pressure ulcer for my loved one?
Answer: Pain management is essential for healing and dignity. Work with their doctor to establish a regular schedule for prescribed pain medication, rather than waiting for pain to peak. Also, minimizing pressure and careful handling during repositioning and dressing changes are key non-pharmacological strategies.
Key Takeaway: Consistency is everything in pressure ulcer care. Daily skin checks, strict repositioning schedules, meticulous skin care, and good nutrition form an unbreakable chain of prevention. When in doubt, always consult a wound care specialist.

