That fiery sensation in your chest, the sour taste in your mouth, the uncomfortable fullness after a meal—acid reflux is more than just occasional heartburn. For millions, it’s a persistent condition known as Gastroesophageal Reflux Disease (GERD). While reaching for an antacid can offer quick relief, it’s merely a temporary fix that masks the symptoms without addressing the root cause. True, long-term management requires a deeper understanding and a strategic approach to diet, lifestyle, and knowing when professional help is essential.
Understanding the Leaky Valve: Why Reflux Happens
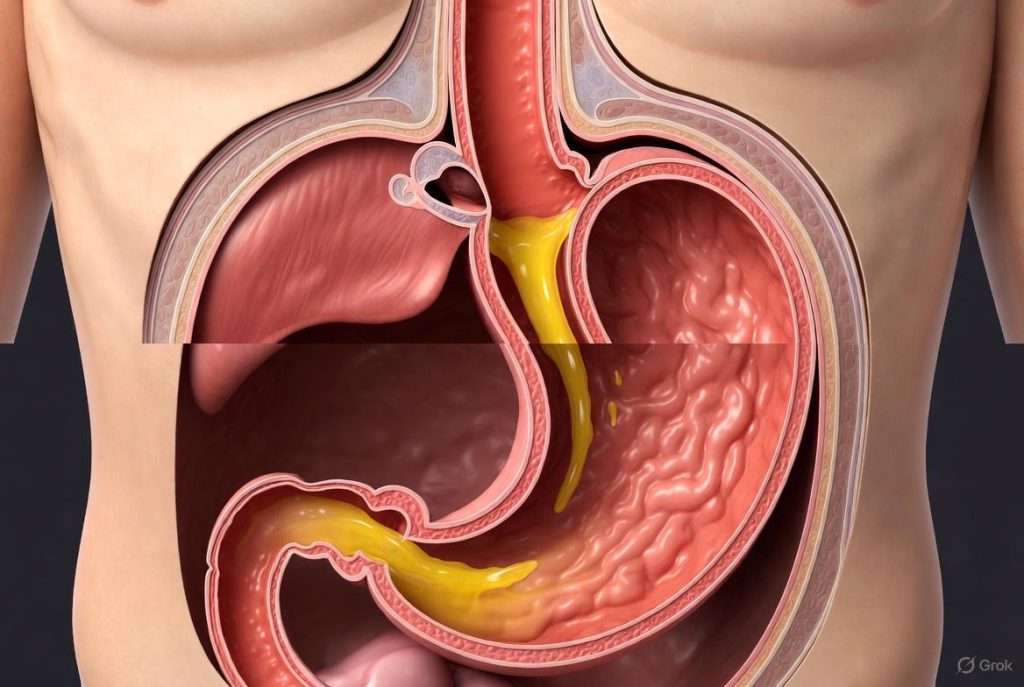
At the entrance to your stomach is a ring of muscle called the lower esophageal sphincter (LES). Think of it as a one-way valve. It’s supposed to open to let food in and then snap tightly shut to prevent stomach acid from washing back up into your esophagus. GERD occurs when this valve becomes weak or relaxes inappropriately.
Chronic exposure to stomach acid can irritate and inflame the esophageal lining (esophagitis), potentially leading to more serious complications like Barrett’s esophagus. The goal of management is to reduce the frequency of these “leaks” and minimize the damage when they occur.
Your First Line of Defense: Identifying Dietary Triggers
Food doesn’t cause the weak valve, but it can be a powerful trigger. What you eat and drink can directly relax the LES, increase stomach acid production, or irritate an already inflamed esophagus. Common culprits include:
· The Classics: Fatty and fried foods, spicy dishes, tomatoes and tomato-based products (sauces, ketchup), citrus fruits and juices, chocolate, and onions.
· The Relaxers: Caffeine (coffee, tea, soda), alcohol, and peppermint can relax the LES.
· The Irritants: Carbonated beverages (the bubbles increase pressure in the stomach) and highly acidic foods can directly sting the esophagus.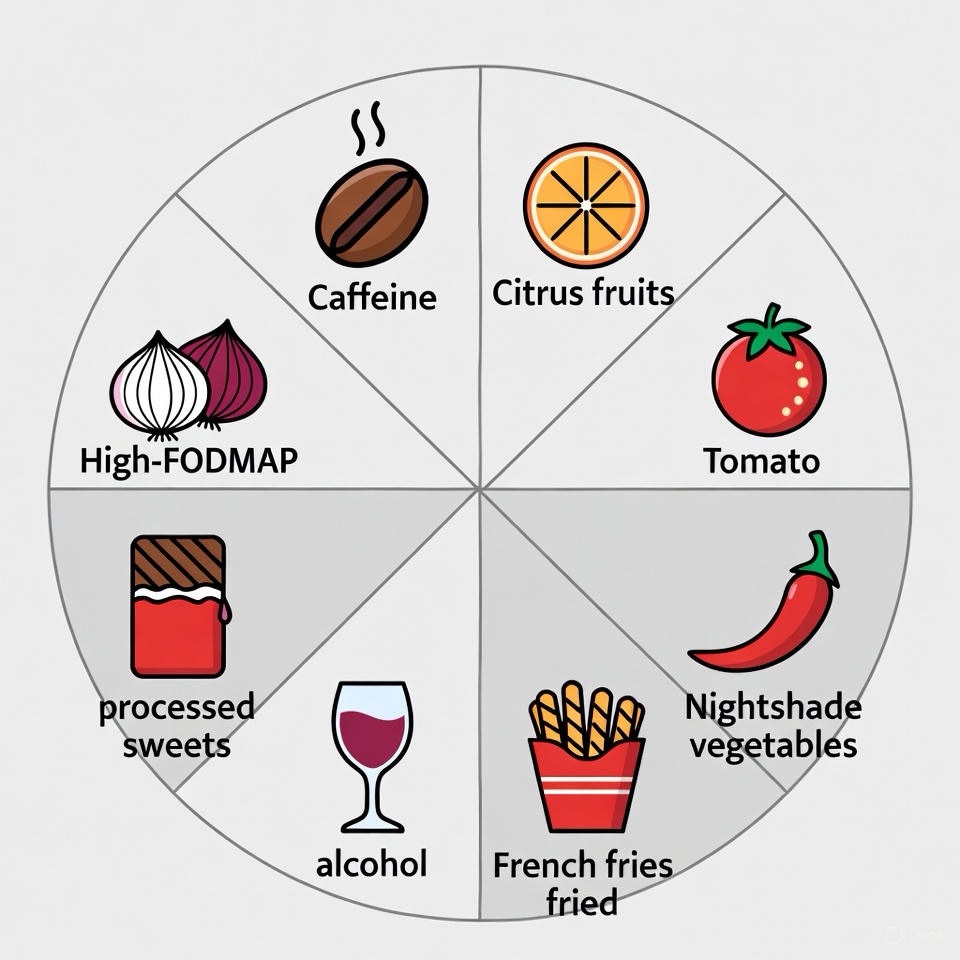
Your Action Plan: Keep a detailed Food & Symptom Diary for two weeks. Note what you eat, when you eat it, and any symptoms that follow. Patterns will emerge, allowing you to personalize your diet. The key is not to eliminate everything, but to identify your specific triggers through trial and elimination.
The Power of Lifestyle Modifications: More Than Just Diet
How and when you live can be as impactful as what you eat. These strategies aim to reduce pressure on the LES and use gravity to your advantage.
1. Master the Art of “How to Eat”:
· Portion Control: Large meals distend the stomach, putting upward pressure on the LES. Opt for smaller, more frequent meals.
· Eat Slowly and Chew Thoroughly: This kick-starts digestion and prevents overloading your stomach.
· The 3-Hour Rule: Avoid lying down for at least 2-3 hours after eating. No late-night snacks!
2. Optimize Your Sleep Environment:
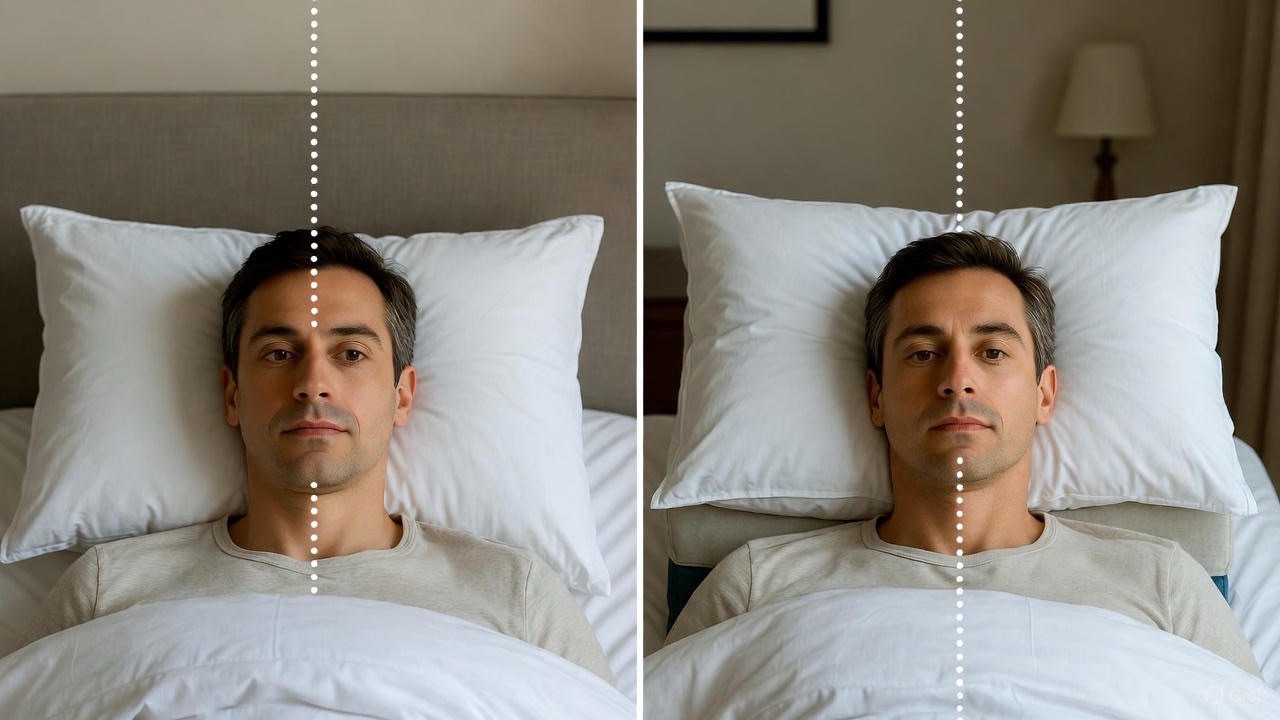
· Elevate the Head of Your Bed: Use bed risers or a wedge pillow under your mattress (not just regular pillows, which can crunch your abdomen). A 6-8 inch elevation lets gravity work overnight.
3. Mind Your Body:
· Weight Management: Excess weight, especially around the abdomen, increases intra-abdominal pressure, forcing stomach contents upward.
· Quit Smoking: Nicotine relaxes the LES and impairs saliva production (saliva helps neutralize acid).
· Wardrobe Wisdom: Avoid tight-fitting clothing, belts, and shapewear that squeeze your midsection.
4. Reconsider Exercise Timing and Type: Avoid vigorous exercise, heavy lifting, or inversions (like yoga poses) immediately after eating. Low-impact activities like walking are better choices post-meal.
When Antacids and Lifestyle Aren’t Enough: Seeking Medical Help
Persistent GERD is not something to ignore. See a doctor if you experience:
· Symptoms occurring more than twice a week.
· Difficulty swallowing or a sensation of food getting stuck.
· Unexplained weight loss.
· Chronic cough, hoarseness, or asthma-like symptoms (silent reflux).
· Symptoms that persist despite over-the-counter medications (like H2 blockers or PPIs) taken as directed for more than two weeks.
· Chest pain, especially if it’s severe or radiates to your arm or jaw—seek immediate medical attention to rule out heart issues.
A doctor can provide a proper diagnosis, which may involve:
· Prescription Medications: Stronger proton pump inhibitors (PPIs) or other drugs to heal the esophagus.
· Diagnostic Testing: An endoscopy allows a doctor to visually examine your esophagus and stomach for damage, or a pH monitoring test to measure acid exposure over 24 hours.
· Discussion of Procedures: For severe, medication-resistant cases, surgical options like fundoplication (wrapping the top of the stomach around the LES to strengthen it) may be considered.
Building Your Long-Term Strategy
Managing GERD is a marathon, not a sprint. It’s about building a sustainable toolkit:
1. Identify and avoid your personal dietary triggers.
2. Integrate key lifestyle habits like mindful eating and sleep elevation.
3. Use medications wisely—PPIs are effective for healing but are best used under a doctor’s guidance for the shortest effective duration.
4. Partner with your healthcare provider for monitoring and to prevent complications.

By moving beyond the quick fix of antacids and adopting a proactive, multi-faceted approach, you can extinguish the fire of reflux for good and reclaim comfort and peace of mind.
FAQs
1. What’s the difference between heartburn, acid reflux, and GERD?
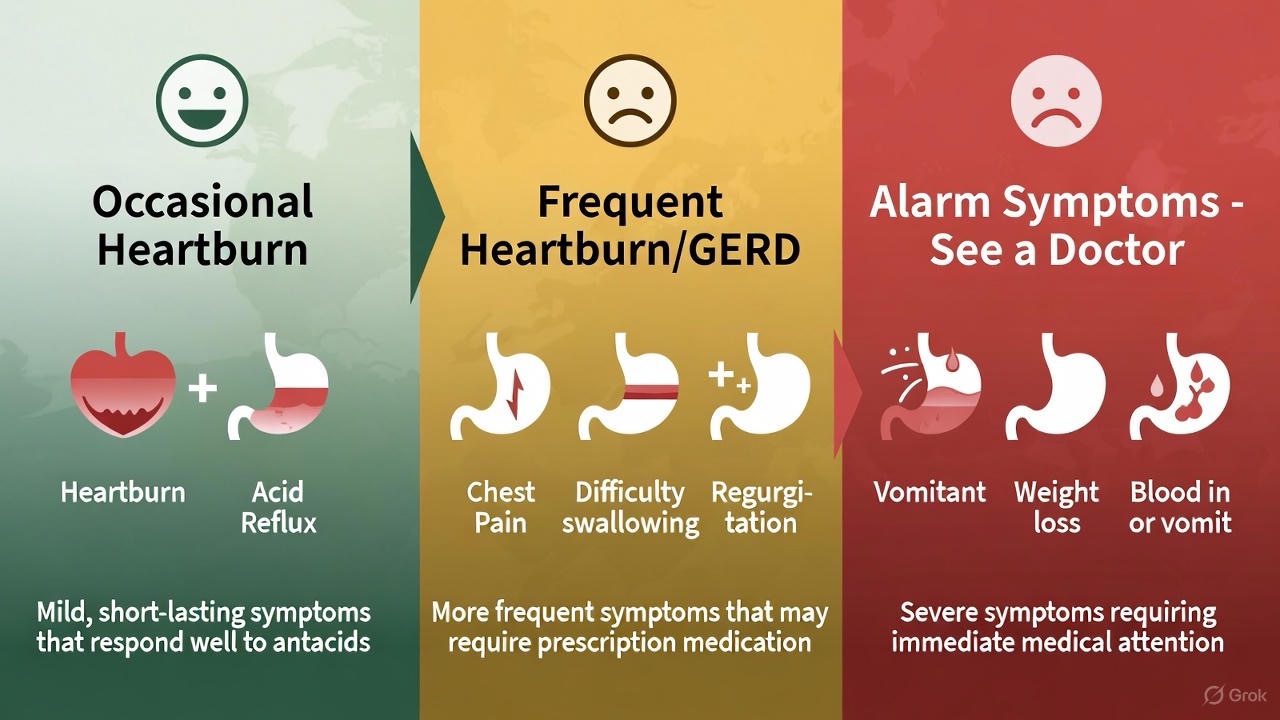
Answer: These terms describe a spectrum of severity:
· Heartburn: The symptom—that burning sensation in your chest caused by stomach acid irritating the esophagus.
· Acid Reflux: The event—the actual backward flow of stomach acid into the esophagus.
· GERD (Gastroesophageal Reflux Disease): The chronic condition—diagnosed when acid reflux occurs two or more times a week or causes inflammation in the esophagus. GERD is frequent, persistent acid reflux.
2. Are over-the-counter antacids (like Tums) or PPIs (like Prilosec) safe for long-term use?
Answer:
· Antacids (Tums, Rolaids): Safe for occasional, infrequent use. Long-term daily use can lead to side effects like diarrhea, constipation, or mineral imbalances.
· PPIs/H2 Blockers (Prilosec OTC, Pepcid): These are for short-term management (typically 14 days for OTC labeling). Using them for months or years without a doctor’s supervision can be associated with risks like nutrient deficiencies (B12, magnesium), increased infection risk, and bone health concerns. Never self-medicate long-term; consult a doctor for persistent symptoms.

3. I already eat a healthy diet. Why do I still have GERD?
Answer: Diet is only one trigger. GERD can be driven by non-diet factors:
· A structurally weak lower esophageal sphincter (LES).
· A hiatal hernia (where part of the stomach pushes into the diaphragm).
· Delayed stomach emptying.
· High intra-abdominal pressure from obesity, tight clothing, or certain exercises.
· Stress, which can increase acid production and perception of pain.
This is why seeing a doctor for a proper diagnosis is crucial.
4. Is drinking alkaline water or milk good for acid reflux?
Answer:
· Alkaline Water: May provide temporary, superficial relief by neutralizing acid in the esophagus, but it does not stop the reflux itself or heal damage. It is not a cure.
· Milk: Provides a fleeting soothing sensation, but its fat and protein content can actually stimulate more acid production shortly after, potentially making things worse. It’s not a recommended remedy.
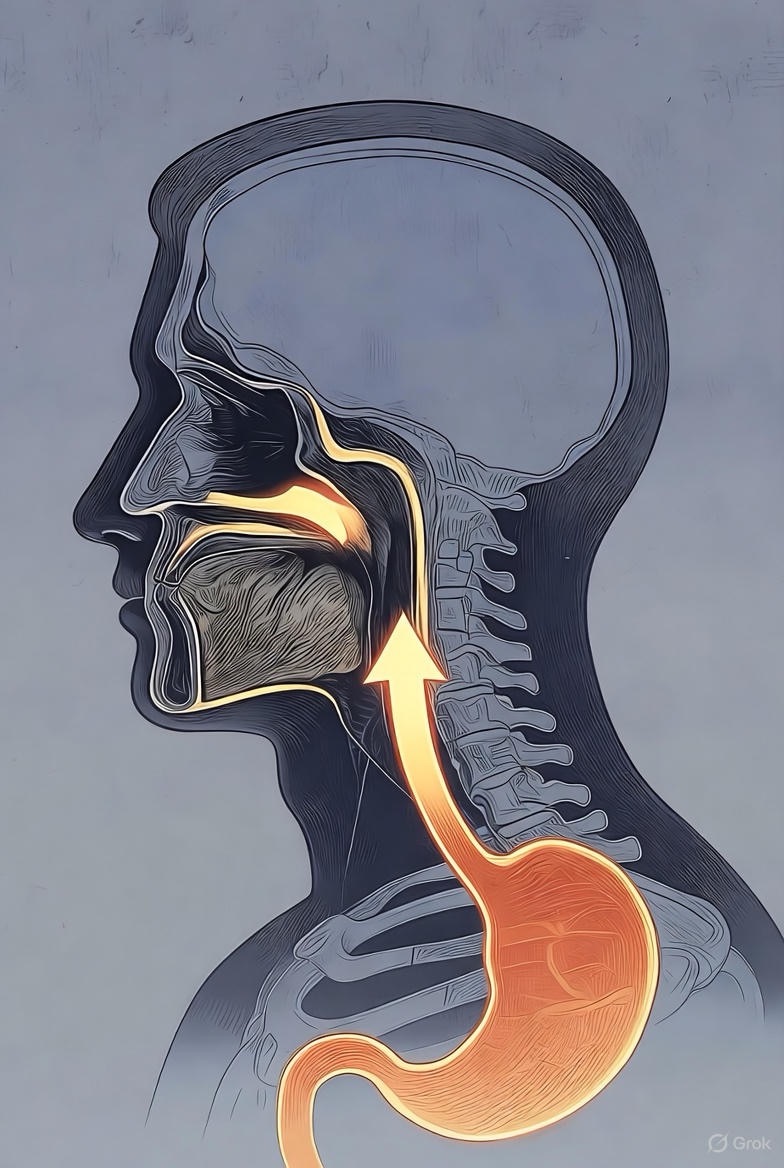
5. What is “silent reflux” (LPR)?
Answer: Laryngopharyngeal Reflux (LPR) is when stomach acid reaches the voice box (larynx), throat, or even the nasal passages. The classic “heartburn” is often absent. Symptoms include:
· Chronic cough or throat clearing
· Hoarseness or a lump-in-the-throat sensation
· Post-nasal drip
· Difficulty swallowing
It requires specific diagnosis and treatment, often with longer-term medication and even stricter dietary changes.
6. Can GERD be cured, or is it just managed?
Answer: For most, GERD is a chronic condition that is effectively managed, not cured. Lifestyle and dietary changes can control symptoms completely for some. For others with a structural issue (like a large hiatal hernia), surgical procedures (like fundoplication) can provide a long-term “cure” by repairing the valve mechanism. Medication controls acid but doesn’t fix the leaky valve.
7. Are there any “good” foods that can help?
Answer: While no food “cures” GERD, some may be less triggering or helpful:
· High-fiber foods: Whole grains, vegetables (non-tomato based), and oatmeal can promote digestive health.
· Alkaline/low-acid foods: Bananas, melons, cauliflower, fennel.
· Lean protein: Skinless poultry, fish.
· Ginger: Has natural anti-inflammatory properties (consume as a mild tea, not spicy ginger ale).
The key is personalization via a food diary.

8. I have night-time reflux. Will propping up on pillows help?
Answer: Standard pillows that just lift your head are insufficient and can even crunch your abdomen, worsening pressure. The goal is to elevate your entire upper body from the waist up. The most effective methods are:
1. Using bed risers under the legs at the head of your bed.
2. A bed wedge pillow that goes under your mattress or on top of it, providing a gradual slope.
Aim for a 6-8 inch elevation.
9. When is acid reflux a sign of something serious?
Answer: Seek immediate medical evaluation for these “alarm symptoms”:
· Difficulty swallowing (dysphagia) or painful swallowing (odynophagia).
· Feeling of food getting stuck in your chest or throat.
· Unintentional weight loss.
· Persistent vomiting or vomiting blood.
· Black, tarry stools (indicating digested blood).
These can signal complications like esophagitis, strictures, or Barrett’s esophagus.
10. Can stress and anxiety really cause GERD?
Answer: Yes, absolutely. Stress doesn’t directly cause the leaky valve, but it can:
· Increase stomach acid production.
· Heighten your perception of pain and discomfort.
· Lead to behaviors that trigger reflux (like poor eating habits, alcohol use, smoking).
Incorporating stress-reduction techniques (mindfulness, yoga, walking) is a key part of a holistic management plan.
11. What’s the connection between weight and GERD?
Answer: Excess weight, particularly abdominal fat, increases intra-abdominal pressure. This constant pressure pushes upwards on the stomach and the LES, forcing it open. Even a modest weight loss of 5-10% of body weight can dramatically reduce reflux frequency and severity.

12. What can I expect if my doctor recommends an endoscopy?
Answer: An upper endoscopy is a common, outpatient procedure. You’ll be sedated. A thin, flexible tube with a camera is passed down your throat to:
· Visually inspect the lining of your esophagus, stomach, and duodenum.
· Check for inflammation, ulcers, or a hiatal hernia.
· Take small tissue samples (biopsies) to test for Barrett’s esophagus (a pre-cancerous change) or other conditions.
It is the gold standard for diagnosing the physical damage caused by GERD.