A small cut, a surgical incision, or a chronic wound like a diabetic foot ulcer—most of us will deal with a wound at some point. While the body is remarkably skilled at healing itself, sometimes bacteria breach our defenses, turning a simple injury into a serious health threat.
Knowing how to spot the early signs of infection can mean the difference between a quick recovery and a dangerous medical emergency. This article will walk you through the 7 critical signs of infection you should never ignore.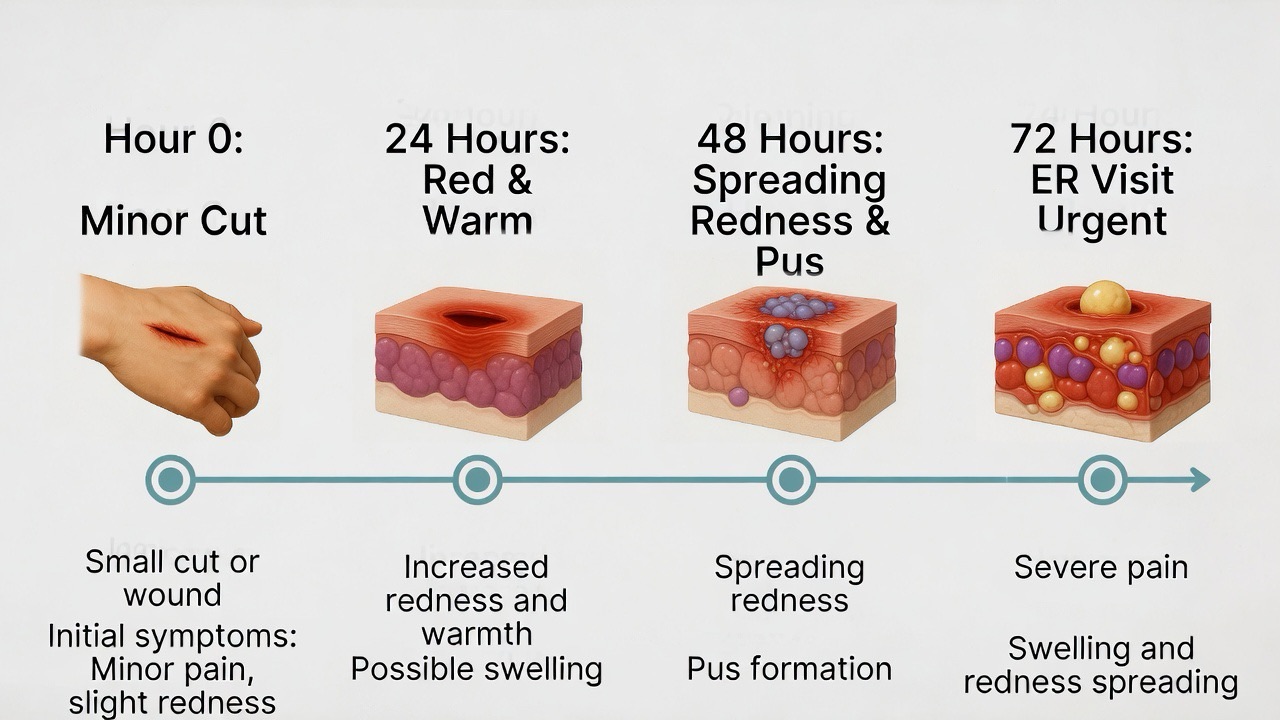
Why Ignoring a Wound Infection is Dangerous
A localized infection can quickly spread to deeper tissues (cellulitis), enter your bloodstream (sepsis), or affect your bones (osteomyelitis). For individuals with diabetes, poor circulation, or compromised immune systems, the risks are even higher. Early recognition and treatment are your best defense.
The 7 Critical Signs of Infection
Monitor your wound closely as it heals. Look for the following warning signs, which are often remembered by the acronym “HOTSPAS.”
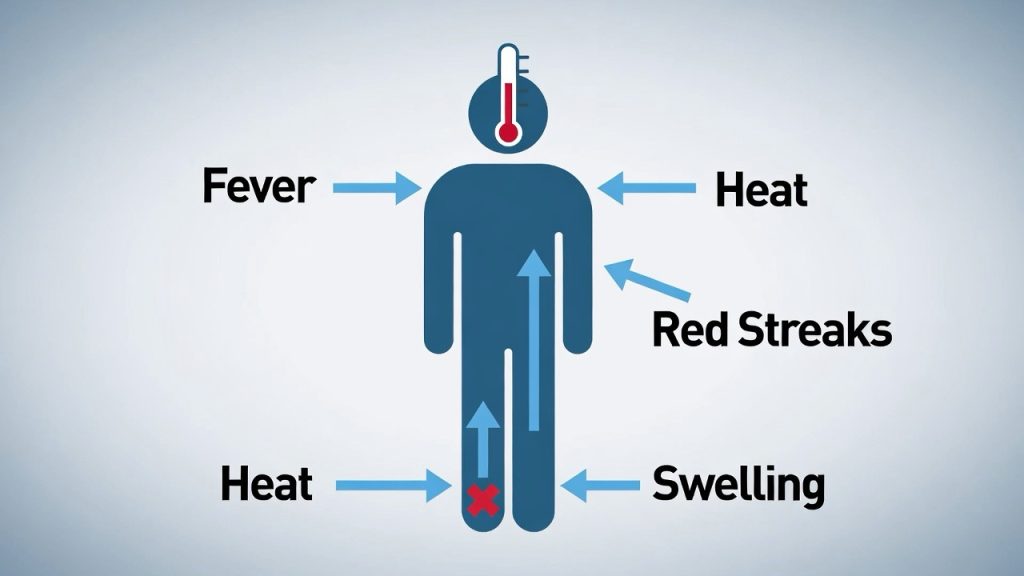
1. Heat
The area around the wound feels noticeably warmer or hot to the touch compared to the surrounding skin. This is caused by increased blood flow as your body sends immune cells to fight the invading bacteria.
2. Oozing or Pus
Increased or new drainage is a major red flag.
· Watch for: Pus, which can be white, yellow, green, or even brown. The drainage may be thick or thin and can sometimes have a foul odor. A small amount of clear or slightly pink fluid is normal; copious or purulent discharge is not.
3. Throbbing or Increasing Pain
While some pain is normal initially, it should gradually improve. A sign of infection is pain that worsens over time, becomes throbbing, or feels like a deep ache or pressure.
4. Swelling & Redness
Some initial redness (extending about a quarter-inch from the wound edge) and swelling are normal. Danger signs include:
· Redness that is spreading or streaking outward (red streaks up your limb are a medical emergency).
· Swelling that is increasing after the first 2-3 days.
5. Pungent Smell
A mild odor can be normal, especially as dressings are changed. However, a strong, foul, or rotten smell emanating from the wound is a classic sign of bacterial infection and tissue breakdown.
6. A Fever
A systemic sign that the infection may be spreading. If you develop a temperature of 100.4°F (38°C) or higher, chills, or general malaise, your body is signaling a fight that requires medical backup.
7. Sick Feeling & Delayed Healing
This encompasses broader systemic symptoms:
· Feeling generally unwell, fatigued, or nauseous.
· The wound shows no signs of progress (getting smaller, forming new tissue) after a week, or it appears to be getting larger or deeper.
What to Do If You See These Signs
Do Not Panic, But Do Act Promptly.
1. For Early Signs (Mild Redness, Slight Swelling): Gently clean the wound with mild soap and water. Apply a fresh, clean bandage. Monitor closely for the next 24 hours. If symptoms worsen, proceed to step 2.
2. For Multiple Signs or Worsening Symptoms (Pus, Spreading Redness, Increased Pain):
· Contact your doctor, urgent care, or a wound care clinic immediately. Describe your symptoms clearly.
· Do not apply antibiotic cream (like Neosporin) unless directed by a healthcare professional, as some people have allergic reactions and it may not be the right treatment.
3. Seek EMERGENCY Care if you experience:
· Red streaks radiating from the wound toward your heart.
· High fever (over 101°F) with chills.
· Confusion, dizziness, or rapid heart rate.
· Severe pain that is unmanageable.
· The wound is gaping open or has a foul-smelling, brown/gray discharge (possible sign of a rare but serious necrotizing infection).
Prevention: Your First Line of Defense
The best way to deal with an infection is to prevent it from happening.
· Clean Immediately: Cleanse any break in the skin with mild soap and running water.
· Cover Up: Keep wounds covered with a sterile bandage until a scab forms and skin reseals.
· Change Dressings Daily: Or whenever they become wet or dirty.
· Hands Off: Avoid picking at scabs or touching the wound with dirty hands.
· Know Your Risk: Individuals with diabetes, peripheral artery disease (PAD), or a weakened immune system must be extra vigilant and seek professional wound care early.

The Bottom Line
Your body sends clear signals when something is wrong. Listening to those signals—the heat, the swelling, the pain that won’t quit—is an act of self-care. Don’t dismiss a wound that seems “a little off.” When in doubt, get it checked out. Prompt medical attention can turn a potential crisis into a manageable condition, ensuring your path to healing stays on track.
FAQs
General Signs & Symptoms
Q1: How can I tell the difference between normal healing and an infection?
A: Normal healing shows gradual improvement: reduced pain, shrinking size, and clean pink/red tissue (granulation). An infection shows progression of symptoms: pain increases, redness spreads, swelling worsens, and you may see pus. A key difference is timing—normal healing gets better daily; infection gets worse.
Q2: My wound is red. When does redness become dangerous?
A: Some redness (about ¼ inch from the wound edge) is normal inflammation. Danger signs include:
· Redness that spreads beyond the initial area
· Streaking (red lines moving away from the wound toward your heart)
· Redness accompanied by increasing warmth, pain, or swelling
If redness expands significantly within 24 hours, seek medical care.
Q3: What does “normal” wound drainage look like vs. infected drainage?
A:
· Normal: Small amounts of clear, pale pink, or straw-colored fluid (serous exudate). This should decrease over time.
· Infected: Pus—thick, opaque, yellow, green, gray, or brown discharge. May be foul-smelling. Increased drainage after initial healing has begun is also suspicious.

Specific Concerns & Situations
Q4: My wound has a smell. Does that always mean infection?
A: Not always, but often. A faint, mild odor when changing a dressing can be normal. A strong, foul, rotten, or sweet smell that persists is a red flag for infection, especially if accompanied by other symptoms. Certain bacteria (like Pseudomonas) have distinctive sweet or musty odors.
Q5: I have a fever but my wound looks okay. Could it still be infected?
A: Yes, absolutely. A fever (100.4°F/38°C or higher), especially with chills, can indicate the infection has spread beyond the wound into your bloodstream (sepsis). This is a medical emergency, even if the wound itself doesn’t look dramatically worse. Don’t wait—seek care immediately.
Q6: How quickly can a wound infection become serious?
A: Alarmingly fast. A minor infection can progress to cellulitis (deep tissue infection) within 24-48 hours. Life-threatening sepsis or necrotizing fasciitis (“flesh-eating bacteria”) can develop in a matter of days or even hours if untreated. This is why daily monitoring and prompt action on early signs are crucial.
Treatment & Care Questions
Q7: Should I use hydrogen peroxide or rubbing alcohol on an infected wound?
A: No—this is outdated advice. Hydrogen peroxide and alcohol damage healthy healing cells and can delay recovery. The proper first-aid step is to gently cleanse with mild soap and lukewarm running water, pat dry, apply a thin layer of petroleum jelly or antibiotic ointment (if not allergic), and cover with a clean bandage. For suspected infection, see a doctor.
Q8: Can I treat a wound infection at home with antibiotics from my medicine cabinet?
A: Never. Do not use leftover antibiotics. This can:
· Cause allergic reactions
· Treat the wrong type of bacteria
· Contribute to antibiotic resistance
· Mask symptoms, allowing the infection to worsen
Only use antibiotics prescribed for your current specific infection by a healthcare provider.
Q9: When exactly should I go to the ER vs. waiting for a doctor’s appointment?
Go to the ER or Urgent Care Immediately if you have:
· Red streaks radiating from the wound
· Fever over 100.4°F with chills
· Rapid heartbeat or breathing
· Confusion, dizziness, or lightheadedness
· Uncontrollable pain
· Wound with grayish, foul-smelling discharge or gas bubbles
Schedule a same/next-day doctor visit if you have:
· Increasing pain, redness, or swelling
· New or worsening pus
· A wound that isn’t healing after 1-2 weeks
· No improvement 48 hours after starting prescribed antibiotics

Risk Factors & Prevention
Q10: Are some people more likely to get wound infections?
A: Yes. Higher-risk individuals include those with:
· Diabetes (especially with poor blood sugar control)
· Poor circulation (PAD, venous insufficiency)
· Weakened immune systems (cancer treatment, HIV, immunosuppressants)
· Obesity
· Nutritional deficiencies
· A history of smoking
Q11: How can I prevent my wound from getting infected from the start?
A: Practice the “Clean, Cover, Check” method:
1. Clean gently with soap and water immediately after injury.
2. Cover with an appropriate bandage; keep it clean and dry.
3. Check daily for the warning signs listed above.
4. Never pick at scabs or healing tissue.
5. Control underlying conditions like diabetes.
Q12: My surgical incision is infected. Did I do something wrong?
A: Not necessarily. While proper aftercare is vital, surgical site infections (SSIs) can occur despite perfect care due to factors like bacterial exposure during surgery, the complexity of the procedure, or individual health factors. Don’t feel ashamed—but do report it immediately to your surgeon, as SSIs require specific treatment.
Q13: Can an infected wound heal on its own without antibiotics?
A: Very minor, superficial infections might resolve if your immune system is strong, but it’s a risky gamble. Most infections require medical intervention. Without treatment, the infection can spread locally, become chronic, or enter the bloodstream. When in doubt, get it checked out—it’s always safer.