You wait for weeks, rearrange your schedule, and finally, you’re in the exam room. Then, in what feels like an instant, it’s over. You’re back in your car, suddenly remembering the two most important questions you meant to ask.
Sound familiar? You’re not alone. With the average appointment lasting just 15 minutes, it’s easy to leave feeling rushed, unheard, and unclear on the next steps. But you can transform this dynamic. By walking in prepared, you become a proactive partner in your care, ensuring your concerns are addressed and your time is used effectively. This checklist is your blueprint.
The Goal: From Passive Patient to Active Partner
Modern healthcare works best as a collaboration. Your doctor brings medical expertise, but you are the expert on your own body and experience. Preparation bridges these two realms, leading to more accurate diagnoses, clearer communication, and better health outcomes.
Step 1: Before the Appointment (The Foundation)
1. Define Your “Chief Concern.”
Ask yourself: “If I could only get one thing addressed today, what would it be?” This is your primary, non-negotiable item. Be specific. Instead of “my knee hurts,” try “I have a sharp pain on the inside of my left knee that starts after 10 minutes of walking.”
2. Create a “Top 3” List.
Realistically, 15 minutes often allows for 1-2 concerns. Prioritize your top three questions or symptoms. Lead with your chief concern. This gives your doctor a clear agenda.
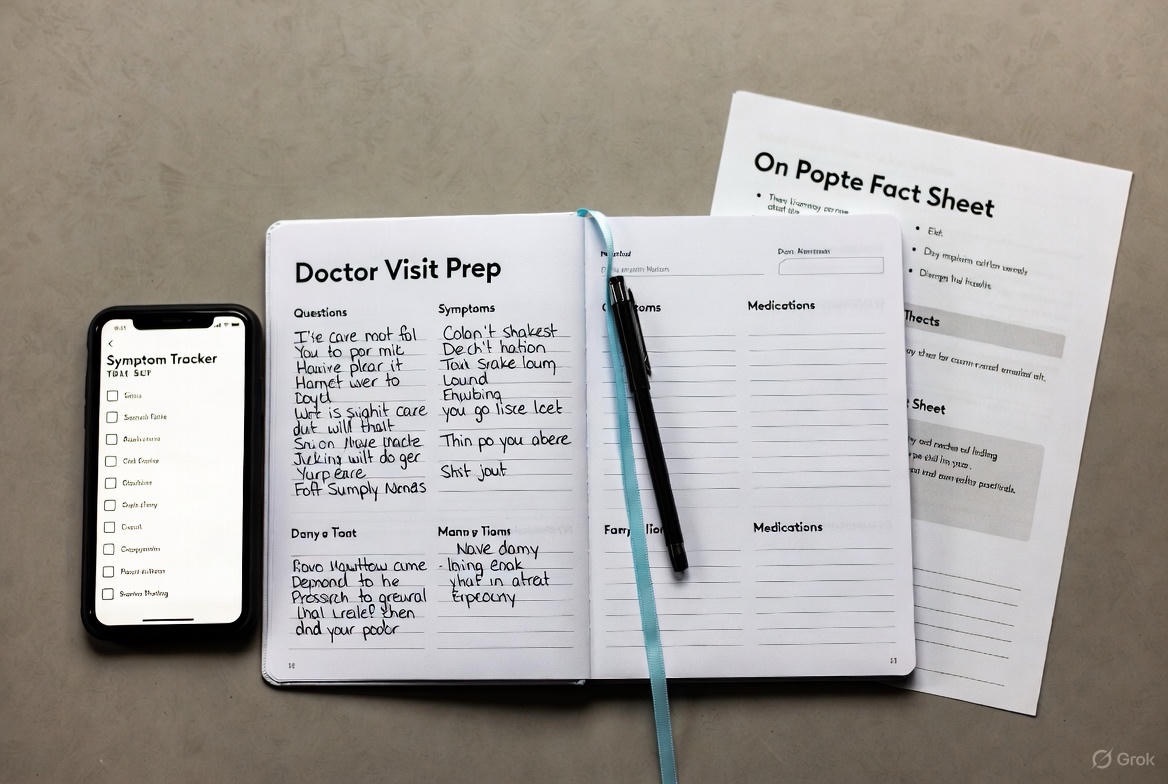
3. Gather Your Data: The Fact Sheet.
Create a one-page summary to hand to your doctor or reference. Include:
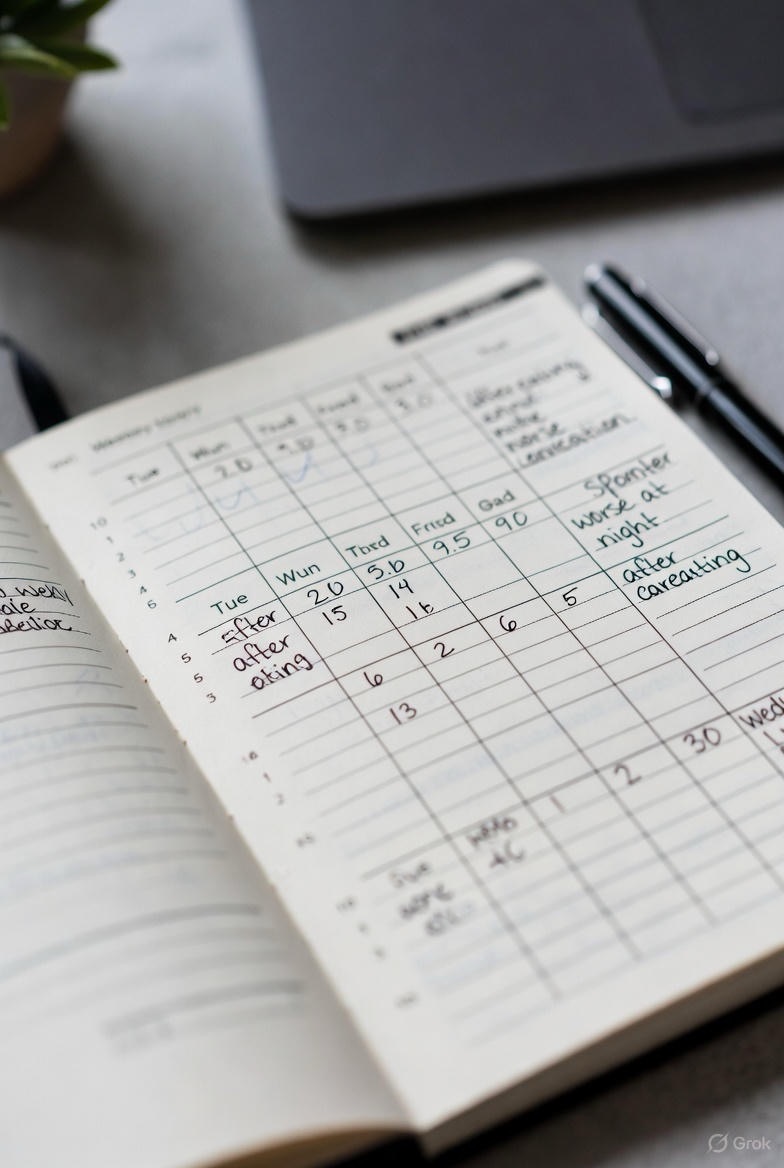
· Symptom Log: What, where, when, how severe? (e.g., “Headache, right temple, every afternoon for 2 weeks, severity 7/10.”) Use the SOAP method: Subjective (how it feels), Objective (observable facts), Aggravating/Alleviating factors, Pattern/Progression.
· Current Medications & Supplements: Names, exact dosages, and frequency. Include over-the-counter drugs, vitamins, and herbs.
· Personal Medical History: Major illnesses, surgeries, and chronic conditions.
· Relevant Family History: Especially for parents or siblings (e.g., heart disease, diabetes, cancer).
· Allergies: Medication, food, or environmental.
4. Bring Your “Evidence.”
If relevant, bring:

· Photos of rashes, swelling, or injury progression.
· A short video of a tremor, gait issue, or child’s symptom that may not appear in the office.
· A food or symptom diary from an app or notebook.
· Recent test results from other providers.
5. Know Your “Why.”
What is your goal for this visit? Is it a diagnosis? Pain management? A referral to a specialist? Understanding a treatment plan? Knowing your desired outcome guides the conversation.
Step 2: During the Appointment (The Collaboration)
6. Start Strong.
Begin the conversation by stating your agenda. “Thank you for seeing me today. I really want to focus on three things: my knee pain, the dizziness I’ve been having, and a review of my blood pressure medication.” This sets expectations immediately.
7. Share Your Fact Sheet.
Hand over your one-page summary. It saves time, ensures accuracy, and lets your doctor scan for key information.
8. Use the “Ask-Share-Ask” Method.
· Ask: Pose your question. (“What could be causing this fatigue?”)
· Share: Provide your relevant data from your fact sheet. (“I’ve noticed it’s worst in the afternoons, and I’m sleeping 8 hours but not feeling rested.”)
· Ask Again: Clarify. (“Given that, could it be related to my thyroid, or are there other causes we should explore?”)

9. Don’t Minimize or Apologize.
Your concerns are valid. Avoid leading with “This is probably nothing, but…” or “I’m sorry to bother you with this.” You are there for care, not validation.
10. Repeat Instructions & Ask for Clarification.
Medical jargon can be confusing. Use the “teach-back” method: “So I want to make sure I understand correctly. I’m to take the new medicine once a day with breakfast, and stop the old one on Sunday, correct?”
11. Ask These Crucial Follow-Up Questions:
· “What is the most likely diagnosis?”
· “What are the other possibilities we should rule out?”
· “What are the next steps? (Tests, referrals, lifestyle changes)”
· “When and how should I expect to see improvement?”
· “What side effects should I watch for with this new medication/treatment?”
· “When and for what reasons should I contact you or seek urgent care?”
Step 3: After the Appointment (The Follow-Through)
12. Take Notes.
Jot down key points during or immediately after the visit. Better yet, bring a companion to listen and take notes for you—it’s incredibly effective.

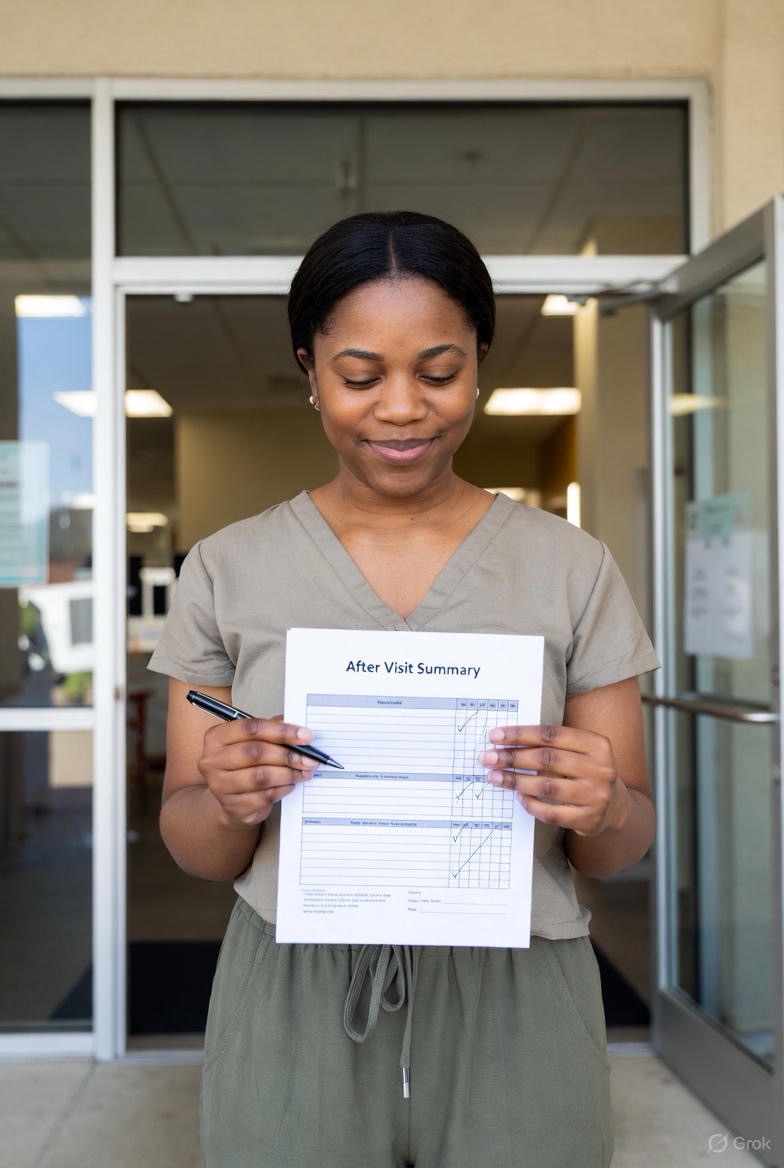
13. Understand Your After-Visit Summary.
Most electronic health records provide a printed or digital summary. Review it before you leave the office. Ensure the listed diagnosis, instructions, and plan match your understanding.
14. Schedule the Next Step Before You Leave.
If you need a follow-up appointment, a blood test, or a referral, try to schedule it on the spot at the front desk. This bypasses future phone tag.
15. Advocate for Yourself.
If you leave feeling dismissed or confused, it’s okay to seek a second opinion. A good doctor will respect a patient who is engaged in their own care
Your 15-minute checklist doesn’t end the conversation—it starts a more productive one. By investing a small amount of time in preparation, you empower yourself, maximize precious time with your doctor, and take a decisive step toward better health. You are the most important member of your healthcare team. Walk into that room ready to lead the meeting.
FAQs
Q1: What if my doctor seems rushed or dismissive when I bring my list?
A: How you frame your list is key. Instead of just handing it over, be proactive:
· Start positively: “I know your time is limited, so I’ve prepared a one-page summary to make our time efficient today.”
· Prioritize clearly: “I have three main concerns. Can we start with #1?”
· If dismissed: Politely but firmly restate: “This [symptom] is really impacting my daily life, and I’d appreciate it if we could explore it today.” A good doctor will respond to respectful assertiveness.
Q2: Is it really okay to bring someone with me? Won’t the doctor think I’m incapable?
A: Absolutely. Medical professionals encourage bringing a companion. They can:
· Serve as a “second set of ears” to remember details you might miss.
· Help describe symptoms objectively if you’re anxious or in pain.
· Take notes so you can focus on the conversation.
Simply introduce them: “This is my [partner/daughter/friend], who’s here to help me remember everything we discuss.”
Q3: How specific do I need to be with symptoms? What if I’m not sure how to describe them?
A: Use the OLD CARTS framework for clear description:
· Onset: When did it start?
· Location: Where exactly is it?
· Duration: How long does it last?
· Character: Sharp, dull, throbbing, burning?
· Aggravating/Alleviating: What makes it better/worse?
· Radiation: Does it spread anywhere?
· Timing: Time of day? Constant or intermittent?
· Severity: On a scale of 1-10.
Even saying “I’m not sure how to describe it, but it’s here and feels like…” is helpful.

Q4: What if I have more than 3 issues? Should I book multiple appointments?
A: For multiple chronic or complex issues:
· Call ahead: When booking, ask: “I have several concerns to address. Would a longer appointment be appropriate, or should I schedule two visits?”
· Lead with impact: Start with what affects your life most. “While I have several things to discuss, my joint pain is preventing me from working, so that’s my priority today.”
· Be realistic: “I know we may not get to everything today. Can we at least address #1 and #2, and schedule a follow-up for the rest?”
Q5: How do I ask for a second opinion without offending my current doctor?
A: Frame it as seeking clarity, not criticism.
· Use collaborative language: “I want to be confident in our treatment plan. Would you recommend getting a second opinion from a specialist?”
· Focus on your needs: “I’d feel more comfortable exploring all options before starting this treatment. Would you be able to refer me to someone for another perspective?”
· Remember: Quality doctors respect informed patients. It’s your right.
Q6: I get nervous and forget everything. What’s a foolproof method?

A: Use the “Notes in Hand” method:
1. Write questions in large font on paper you can hold.
2. Bring a pen and check off questions as they’re answered.
3. Physically hand your doctor the fact sheet (from Step 1) at the start.
4. Record the visit (with permission): “Would you mind if I record this so I can review it later?” Most smartphones have a voice memo app.
Q7: What should I do if I don’t understand the medical terms my doctor uses?
A: Interrupt politely and ask for translation.
· Use exact phrasing: “Could you explain what ‘[medical term]’ means in everyday language?”
· Request analogies: “Is that similar to…?”
· Ask for visuals: “Could you draw or show me a diagram of what you mean?”
· Repeat back: “So what I’m hearing is…” in your own words.

Q8: How do I handle my doctor constantly running late without getting flustered?
A: Prepare for the wait, but also maximize your face time.
· Bring your preparation materials to review while waiting.
· Pack water, a snack, and reading material.
· When you enter, acknowledge gently: “I know you’re running behind today—I appreciate you taking time with me.” This sets a collaborative tone.
· Still stick to your agenda: Their lateness shouldn’t shorten your allocated time once you’re in the room.
Q9: What if my doctor orders tests but doesn’t explain why?
A: Use the “Three Whys” approach:
1. “Why is this test the right one for my symptoms?”
2. “Why now versus waiting?”
3. “What will the possible results mean for my treatment plan?”
Always ask: “What are the next steps once we get the results?”

Q10: How can I ensure my doctor actually reads the forms I filled out beforehand?
A: Use them as a conversation starter.
· Bring an extra copy with you.
· Reference them directly: “As I noted on my intake form, my pain level has been at a 7. Based on that, what do you think…?”
· Highlight: Use a colored marker on one or two key points on your copy to draw attention.
Q11: What if I feel my concerns are being attributed to anxiety or weight without being fully investigated?
A: Advocate using persistent, specific language.
· Acknowledge, then redirect: “I understand that [anxiety/weight] can be a factor. However, these specific symptoms are new/different. Could we rule out other causes first?”
· Request documentation: “Could you note in my chart that I requested further investigation for [specific symptom], and your reason for declining?”
· Be specific about change: “Even though I’ve had this weight for years, this dizziness is new in the last month. What could be causing this change?”
Q12: Is it appropriate to bring research or articles I found online?

A: Yes, if done correctly.
· Be selective: Bring 1-2 reputable sources (like Mayo Clinic, CDC, or major medical journals).
· Frame it as curiosity: “I came across this information and wanted your expert opinion on how it might apply to my situation.”
· Avoid: “I read online that I have…” or presenting stacks of printouts from unvetted sources.
Remember: Preparation transforms anxiety into empowerment. Walking into an appointment with clear questions and organized information isn’t just good for you—it helps your doctor provide the best care possible. You are the CEO of your health; think of your doctor as your most valuable consultant.

