Whether it’s a scraped knee, a surgical incision, or a deeper cut, your body has a remarkable ability to repair itself. Wound healing is one of the most complex and fascinating processes in human biology, involving a carefully orchestrated sequence of events that transform damaged tissue back into functioning skin. Understanding how this process works can help you better care for wounds and recognize when healing isn’t progressing as it should.
What Is Wound Healing?
Wound healing is your body’s natural process of repairing damaged tissue. The moment your skin is broken, your body immediately springs into action, deploying specialized cells, proteins, and growth factors to close the wound, fight infection, and rebuild tissue. This process follows four distinct but overlapping stages, each essential to proper recovery.
The 4 Stages of Wound Healing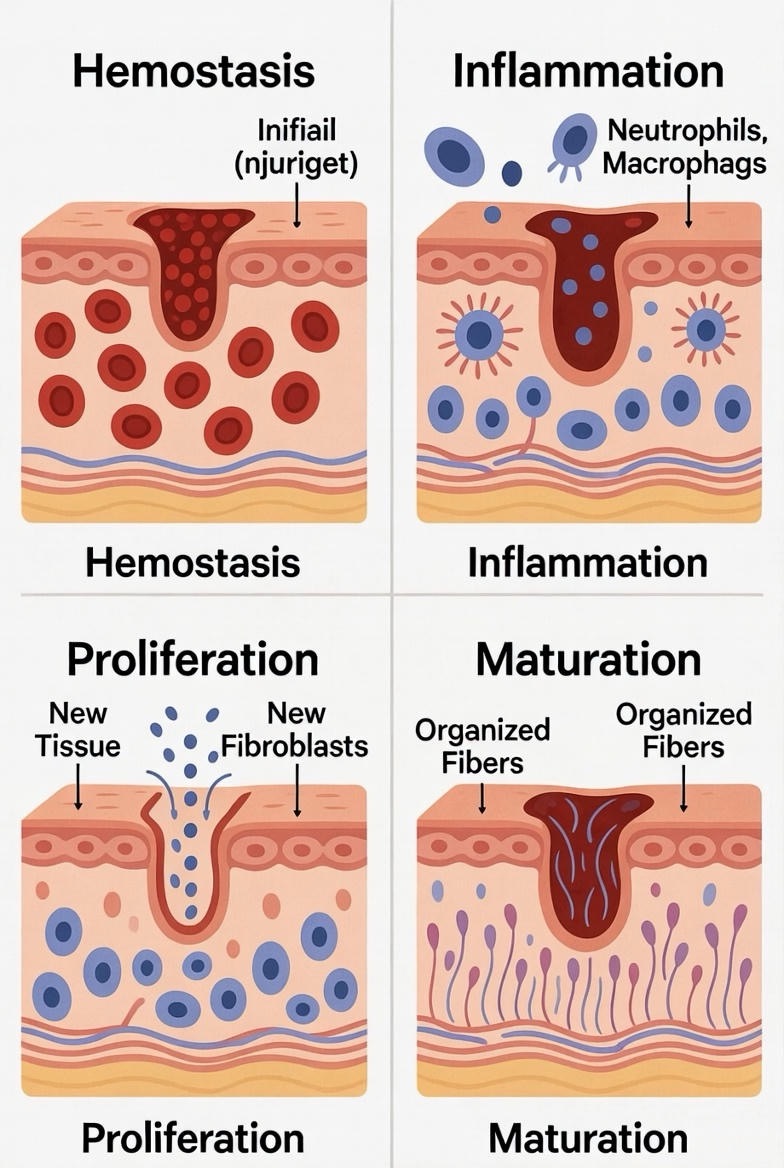
Stage 1: Hemostasis (Immediate to Several Hours)
The healing process begins the instant you’re injured. Hemostasis is your body’s emergency response to stop bleeding and prevent excessive blood loss.
When a blood vessel is damaged, it immediately constricts to reduce blood flow. Platelets, the tiny disc-shaped cells in your blood, rush to the injury site and stick together to form a temporary plug. These platelets also release chemical signals that attract more platelets and activate clotting factors in your blood. Within minutes, a mesh of fibrin proteins forms over the wound, creating the blood clot you see as a scab. This clot not only stops bleeding but also provides a protective barrier against bacteria and creates a temporary scaffold for incoming repair cells.
For minor wounds, this stage typically completes within minutes to hours. The familiar scab that forms is actually a sophisticated biological bandage doing important work beneath the surface.
Stage 2: Inflammation (1 to 5 Days)
Once bleeding stops, inflammation takes over. Despite its bad reputation, inflammation is absolutely essential for proper wound healing.
During this stage, damaged cells and platelets release chemical signals that dilate blood vessels and increase blood flow to the area. This is why wounds become red, warm, and swollen—these are signs your immune system is working. White blood cells, particularly neutrophils and macrophages, flood into the wound to clean house. They destroy bacteria and remove dead tissue and cellular debris, essentially preparing a clean workspace for the next phase of healing.
Macrophages also release growth factors that signal the body to start building new tissue. While inflammation is necessary, excessive or prolonged inflammation can actually impair healing, which is why managing wounds properly is so important.
Stage 3: Proliferation (4 Days to 3 Weeks)
This is the rebuilding phase, where your body works to fill in the wound and cover it with new skin.
Several important processes happen simultaneously during proliferation. Fibroblasts, specialized cells that produce collagen, migrate into the wound and begin laying down new connective tissue. This forms granulation tissue—the pink, bumpy tissue you might see in healing wounds. Meanwhile, new blood vessels sprout and grow into this tissue through a process called angiogenesis, bringing oxygen and nutrients to support healing.
At the edges of the wound, epithelial cells begin to multiply and migrate across the wound surface, gradually closing the gap. This process, called epithelialization, is what eventually covers the wound with new skin. The wound also begins to contract, with specialized cells pulling the edges together to reduce the size of the area that needs to be filled in.
For small wounds, you’ll see significant progress during this stage as the wound closes and begins to look more like normal skin, though it will still be fragile and vulnerable.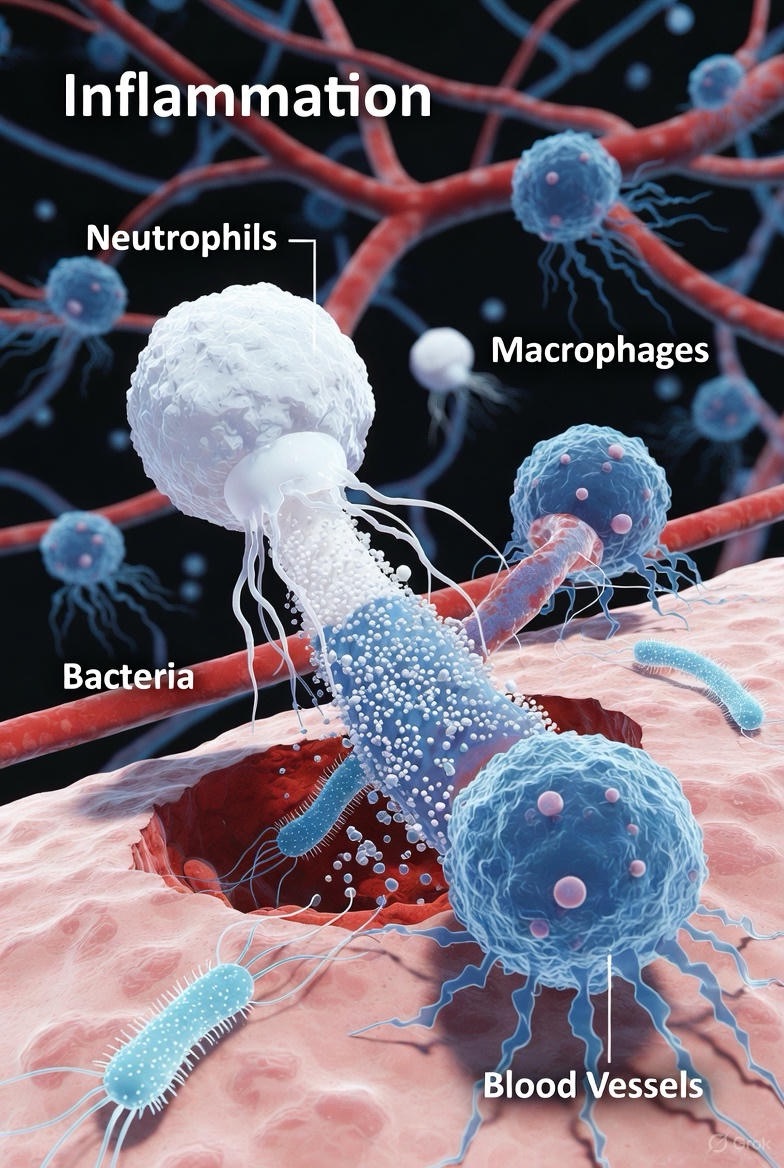
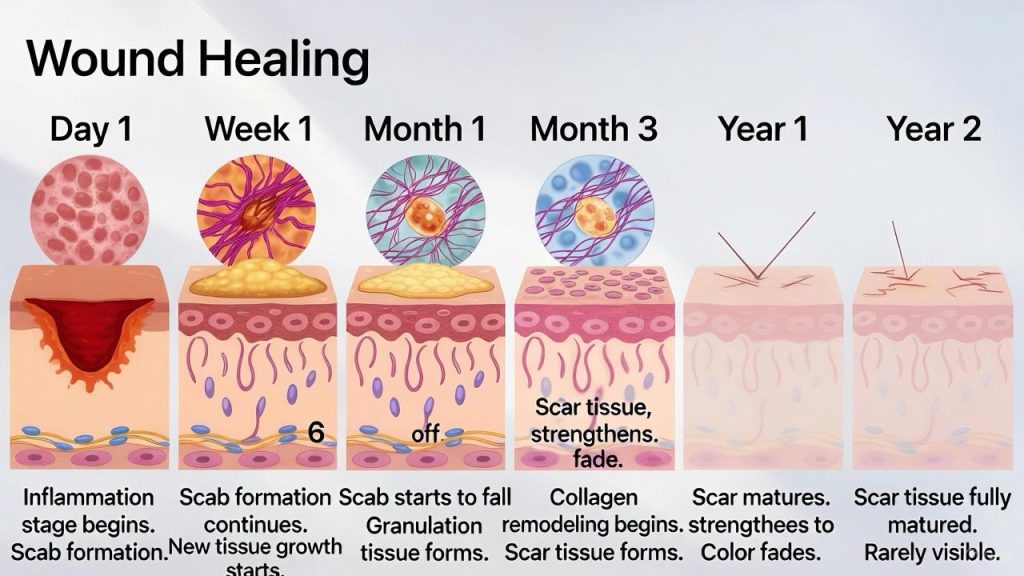
Stage 4: Maturation (3 Weeks to 2 Years)
Also called the remodeling phase, maturation is the longest stage of wound healing, potentially lasting months or even years for larger wounds.
During maturation, the body refines and strengthens the new tissue. The randomly organized collagen laid down during proliferation is gradually replaced with stronger, more organized collagen fibers aligned along tension lines. The wound becomes stronger, though healed skin never quite reaches the full strength of undamaged skin—typically achieving only about 80% of its original strength.
Blood vessels that were formed to support healing but are no longer needed regress, and the red appearance of the scar gradually fades. The tissue continues to remodel, and the scar typically becomes flatter and less noticeable over time, though the extent of scarring varies based on factors like wound size, location, genetics, and how well the wound was cared for during healing.
Factors That Affect Wound Healing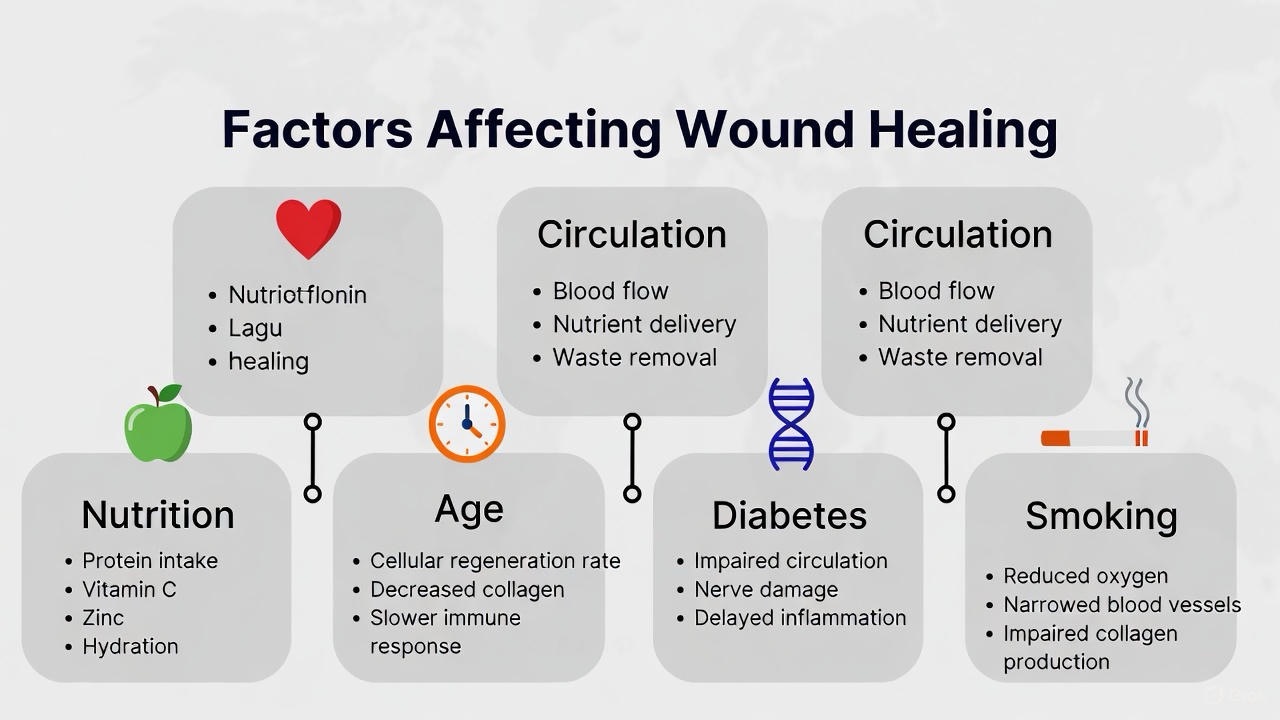
Several factors can speed up or slow down the healing process. Age plays a role, with older adults typically healing more slowly due to reduced cellular activity and circulation. Nutrition is crucial—your body needs adequate protein, vitamins (especially A and C), minerals like zinc and iron, and overall calories to fuel the healing process.
Chronic conditions like diabetes can significantly impair healing by affecting circulation and immune function. Smoking restricts blood flow and reduces oxygen delivery to tissues, dramatically slowing healing. Medications such as corticosteroids and some chemotherapy drugs can suppress the immune system and interfere with healing stages.
Proper wound care, including keeping wounds clean, moist, and protected, supports the natural healing process. Adequate blood flow to the wound site is essential for delivering the cells and nutrients needed for repair.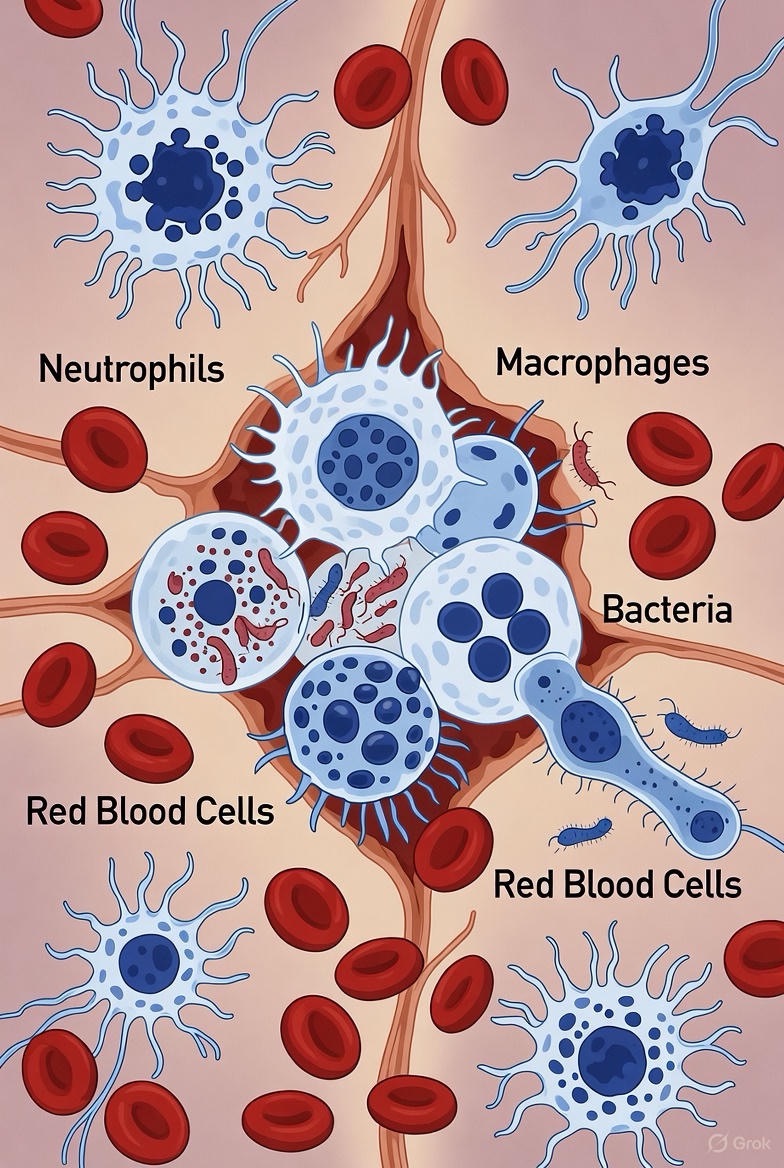
When to Seek Medical Attention
While most minor wounds heal without complications, certain signs indicate you should see a healthcare provider. Watch for increasing pain, redness, or swelling after the first few days, which could signal infection. Pus, increasing warmth, or red streaks extending from the wound are also concerning. Wounds that haven’t begun to heal after two weeks, those with edges that won’t stay together, or injuries accompanied by fever should be evaluated by a medical professional.
Deep wounds, those with jagged edges, animal or human bites, and wounds contaminated with dirt or debris often require professional care to heal properly and minimize scarring.
Supporting Your Body’s Healing
Understanding the wound healing process empowers you to support your body’s natural repair mechanisms. Keep wounds clean and covered, stay hydrated, eat a nutritious diet rich in protein and vitamins, avoid smoking, and manage any chronic health conditions. When in doubt about a wound’s progress, don’t hesitate to consult a healthcare provider.
Your body’s ability to heal itself is truly remarkable. Each stage of wound healing represents millions of years of evolutionary refinement, a biological program written into your cells. By understanding and supporting this process, you can help ensure your wounds heal as quickly and completely as possible.
FAQs
General Wound Healing Questions
Q: How long does it take for a wound to heal completely?
A: The timeline varies significantly depending on the wound’s size, depth, and location. Minor cuts and scrapes typically heal within 1-2 weeks. Deeper wounds may take 3-6 weeks to close and several months to fully strengthen. Surgical incisions generally take 6-8 weeks to heal substantially, though the maturation phase can continue for up to two years. Factors like age, health status, and wound care practices all influence healing speed.
Q: Is it better to keep a wound covered or let it air out?
A: Modern wound care research shows that keeping wounds covered and moist (but not wet) promotes faster healing and reduces scarring. A covered wound maintains optimal moisture levels, protects against bacteria, and creates an ideal environment for cell migration. However, once a wound has formed a stable protective layer, some air exposure can be beneficial. For most wounds, keep them covered during the initial healing stages, especially the first few days.
Q: Should I use hydrogen peroxide or rubbing alcohol on wounds?
A: No, avoid these products on open wounds. While they kill bacteria, they also damage healthy tissue and slow healing. Instead, clean wounds with mild soap and clean water, or use saline solution. For antiseptic needs, products like diluted povidone-iodine or those specifically designed for wound care are gentler and more effective.
Scabs and Wound Appearance
Q: Should I pick off my scab?
A: Absolutely not. Scabs serve as natural bandages that protect healing tissue underneath. Picking scabs introduces bacteria, disrupts the healing process, increases bleeding, and significantly raises the risk of scarring. Let scabs fall off naturally when the skin beneath has healed sufficiently.
Q: Why does my wound itch as it heals?
A: Itching is actually a sign of healing. As new skin cells grow and nerve endings regenerate, they send signals to your brain that register as itching. Additionally, histamine released during the healing process can cause itchiness. The formation of new collagen fibers also stimulates nerve endings. While annoying, itching generally indicates your wound is progressing through the proliferation stage normally.
Q: What does healthy wound healing look like?
A: A healthy healing wound progressively improves. Initially, you’ll see redness and slight swelling around the edges, which should gradually decrease after the first few days. The wound should become smaller over time as edges pull together. Pink or red granulation tissue appearing in the wound bed is a positive sign. Clear or slightly yellow fluid is normal, but thick pus indicates infection. The area should become less painful over time, not more.
Wound Care and Treatment
Q: When do I need stitches?
A: Seek medical attention for stitches if the wound is deeper than 1/4 inch, has edges that gape open and won’t stay together, is located on the face or over a joint, won’t stop bleeding after 10 minutes of direct pressure, or is longer than 1/2 inch. Additionally, any wound caused by a dirty or rusty object, animal bite, or human bite should be professionally evaluated regardless of size.
Q: Can I shower or bathe with an open wound?
A: For most wounds, brief showers are fine after the first 24-48 hours, but avoid prolonged water exposure. Keep the wound covered with a waterproof bandage if possible, pat it dry gently afterward, and reapply a clean dressing. Avoid soaking in bathtubs, hot tubs, or swimming pools until the wound has closed and formed new skin, as prolonged exposure softens tissue and increases infection risk.
Q: What’s the best ointment for wound healing?
A: Plain petroleum jelly (like Vaseline) is highly effective for keeping wounds moist and promoting healing. Antibiotic ointments like bacitracin or Neosporin can help prevent infection in the first few days, though they’re not always necessary for clean, minor wounds. Some people develop allergies to antibiotic ointments, particularly those containing neomycin. For chronic wounds or specific conditions, your doctor might recommend specialized products.
Infection and Complications
Q: How can I tell if my wound is infected?
A: Watch for these warning signs: increasing pain after the first 2-3 days, expanding redness or red streaks radiating from the wound, increasing swelling or warmth, thick yellow or green pus with a foul odor, fever above 100.4°F (38°C), swollen lymph nodes near the wound, or the wound becoming more tender rather than less. If you notice these signs, seek medical attention promptly.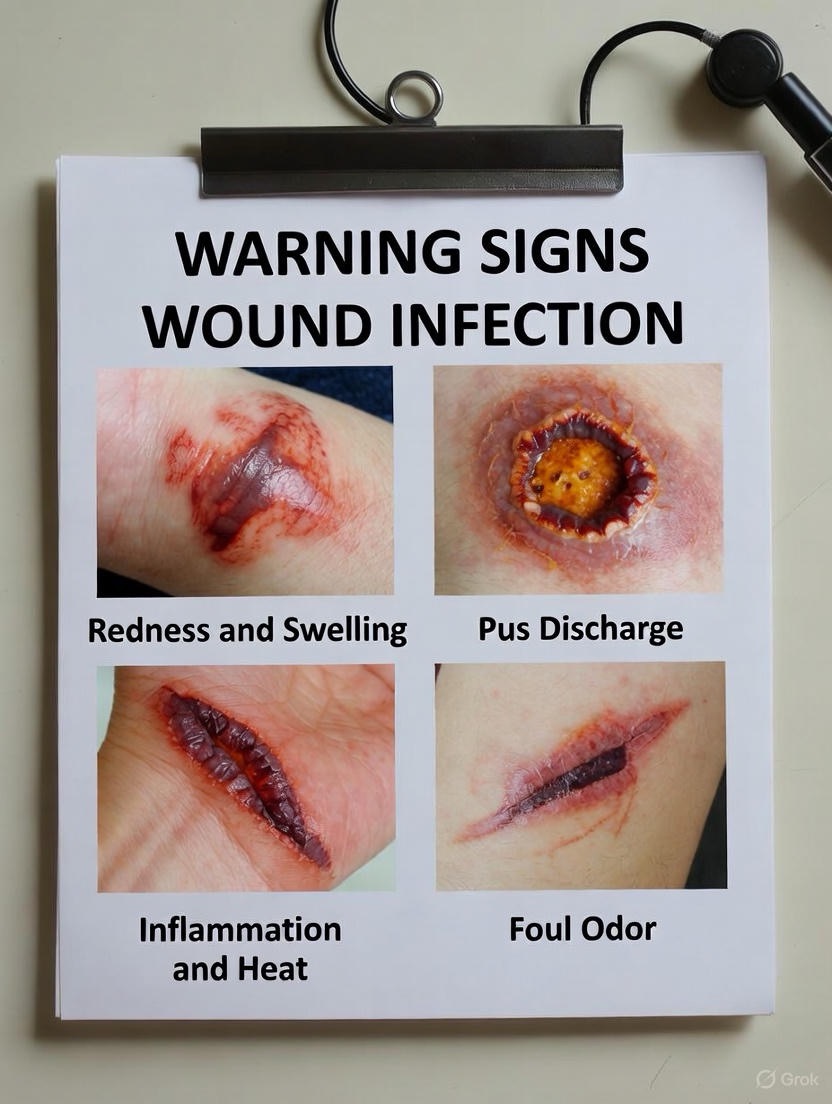
Q: Why isn’t my wound healing?
A: Several factors can delay healing. Poor blood circulation prevents adequate oxygen and nutrient delivery. Diabetes impairs immune function and circulation. Infections consume resources meant for healing. Continued pressure or movement at the wound site disrupts tissue formation. Nutritional deficiencies, particularly protein, vitamin C, and zinc, deprive your body of building blocks. Certain medications, smoking, and advanced age also slow healing. If a wound hasn’t shown improvement after two weeks, consult a healthcare provider.
Q: Can a wound heal without stitches?
A: Yes, many wounds heal well without stitches through secondary intention (healing from the bottom up). However, this typically takes longer, may result in more scarring, and has a slightly higher infection risk. Clean wounds with straight edges that aren’t too deep can often be held together with butterfly bandages or surgical tape. The decision depends on wound characteristics and location.
Scarring
Q: How can I minimize scarring?
A: Several strategies reduce scarring: keep the wound moist during healing, avoid sun exposure on healing wounds for at least a year (UV radiation darkens scars), don’t pick at scabs or healing tissue, massage the area gently once it’s fully closed to improve collagen organization, consider silicone gel sheets or creams once the wound has closed, and ensure adequate nutrition with plenty of protein and vitamin C. Genetic factors play a significant role, but proper care makes a substantial difference.
Q: Will my scar fade over time?
A: Yes, most scars fade significantly. Initially red or purple, scars typically lighten over 12-24 months during the maturation phase. They may become flatter and less noticeable, though they rarely disappear completely. Hypertrophic scars (raised but contained) generally improve more than keloid scars (raised and spreading). Sun protection helps prevent darkening that makes scars more visible.
Special Situations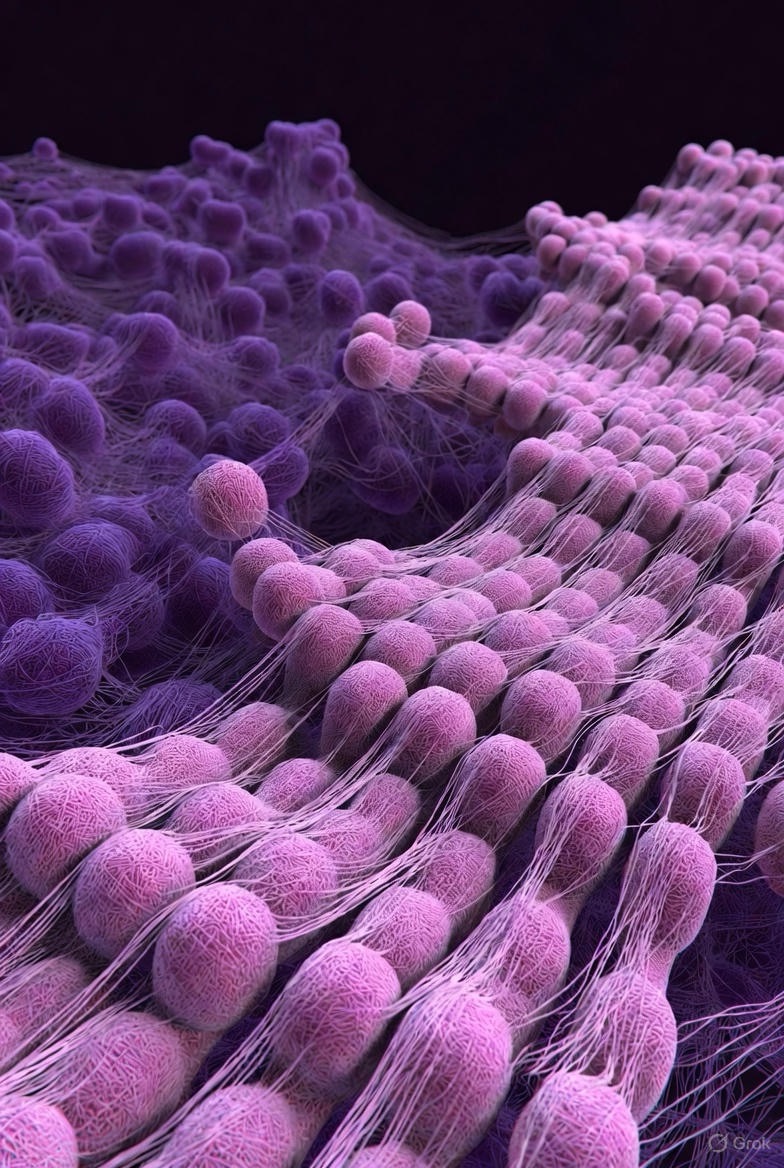
Q: Do wounds heal faster when you sleep?
A: Yes, sleep is crucial for wound healing. Your body produces more growth hormone during deep sleep, which accelerates tissue repair. The immune system functions more effectively with adequate rest, and cellular regeneration peaks during sleep. Studies show that people who sleep poorly heal significantly slower than those who get 7-9 hours of quality sleep nightly.
Q: Does age affect wound healing?
A: Absolutely. As we age, wound healing slows due to several factors: reduced circulation means less oxygen and nutrients reach wounds, decreased collagen production affects tissue strength, thinning skin is more fragile and repairs more slowly, immune function declines with age, and older adults often have chronic conditions that impair healing. While aging slows healing, maintaining good nutrition, hydration, and overall health helps optimize the process.
Q: Can certain foods speed up wound healing?
A: Yes, nutrition directly impacts healing speed. Protein-rich foods (lean meats, fish, eggs, legumes) provide amino acids for tissue building. Vitamin C from citrus fruits, berries, and leafy greens supports collagen formation. Zinc from nuts, seeds, and whole grains aids cell growth. Vitamin A from sweet potatoes, carrots, and spinach supports immune function. Omega-3 fatty acids from fish reduce excessive inflammation. Staying well-hydrated is equally important for cellular function.
Q: Is yellow discharge from a wound normal?
A: It depends. Clear to slightly yellow, thin fluid (serous drainage) is normal during healing. However, thick, cloudy, yellow-green pus with a foul odor indicates infection and requires medical attention. Some yellowish material in the wound bed might be slough (dead tissue), which is a normal part of healing but should gradually decrease. When in doubt about any drainage, have it evaluated by a healthcare professional.
Q: Can stress slow wound healing?
A: Yes, chronic stress significantly impairs healing. Stress hormones like cortisol suppress immune function, reduce blood flow to peripheral tissues, interfere with sleep (which is crucial for healing), and can lead to behaviors that impair healing, like poor nutrition or smoking. Studies show that stressed individuals heal measurably slower than those who are relaxed. Managing stress through relaxation techniques, adequate sleep, and emotional support can positively impact wound healing.