For the millions living with diabetes, a small cut, blister, or callus on the foot is not just a minor inconvenience—it’s a potential medical emergency. Diabetic foot ulcers (DFUs), open sores or wounds that typically occur on the bottom of the foot, are one of the most common and serious complications of diabetes. They affect approximately 15% of diabetics at some point in their lives and are the leading cause of non-traumatic lower limb amputations worldwide.
Yet, there is powerful, hopeful news: The vast majority of diabetic foot ulcers are preventable. Knowledge, vigilance, and a consistent daily routine form the strongest defense. This guide breaks down the causes, teaches you to recognize the earliest warning signs, and provides actionable strategies to protect your feet.
Why Are People with Diabetes at Such High Risk?
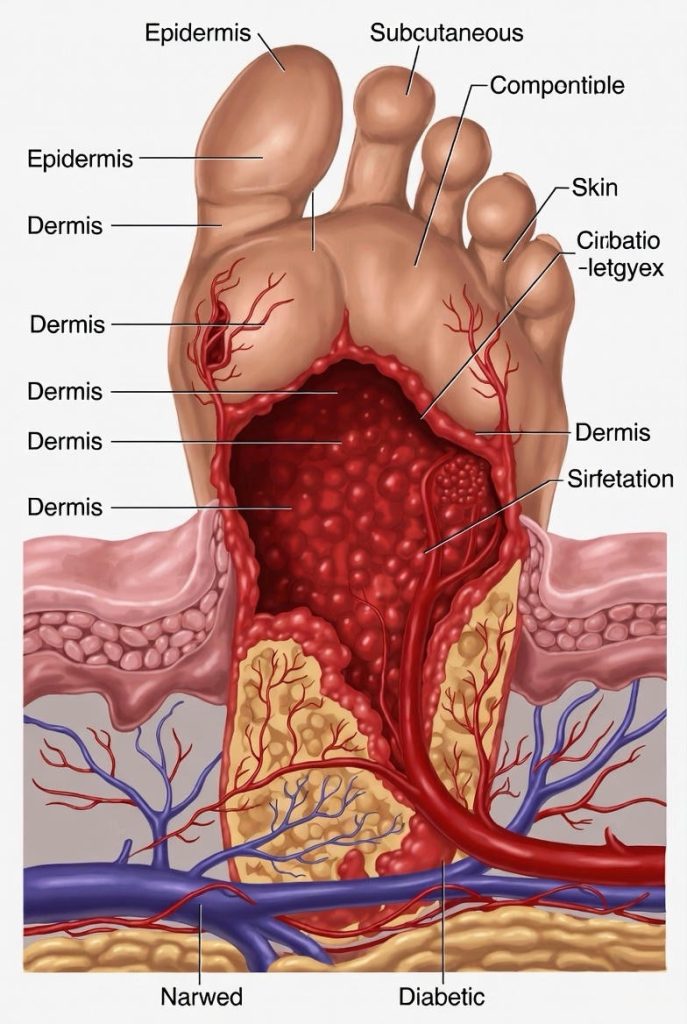
Diabetic foot ulcers don’t happen by chance. They are the result of a perfect storm of three key diabetes-related complications:
1. Neuropathy (Nerve Damage)
High blood sugar levels over time can damage the nerves in your feet—a condition called peripheral neuropathy. This means you lose protective sensation.
· The Consequence: You might not feel a pebble in your shoe, a blister from new footwear, or the heat from a hot bath. A minor injury can go unnoticed, worsen, and become infected without you realizing it.
2. Peripheral Arterial Disease (PAD – Poor Circulation)
Diabetes accelerates the narrowing and hardening of the arteries that supply blood to your legs and feet.
· The Consequence: Poor circulation starves tissues of oxygen and nutrients, making it harder for even a small wound to heal. It also reduces your body’s ability to fight infection.

3. Immune System Impairment
Hyperglycemia can weaken the white blood cells that defend against infection.
· The Consequence: A small break in the skin can quickly become a serious, spreading infection.
Together, these factors create a dangerous cycle: Loss of sensation leads to unrecognized injury. Poor circulation prevents healing. A weakened immune system allows rapid infection.
The Early Warning Signs: Don’t Wait for a Wound
A diabetic foot ulcer is a late-stage event. Catching problems before the skin breaks is the ultimate goal. Look for these early red flags:
· Changes in Skin Color or Temperature: Redness, warmth (a sign of inflammation or infection), or a foot that is cooler than the other (a sign of poor circulation).
· Swelling: In the foot or ankle, which can indicate poor circulation or infection.
· New or Unusual Pain: While neuropathy often causes numbness, some experience aching, cramping, tingling, or burning pain.
· Changes in Skin Texture: Dry, cracked skin (especially on heels), calluses, or corns. Note: Never try to cut these yourself.
· Drainage: Any fluid or blood staining on your socks.
· Odor: Any foul smell coming from the foot.
· Changes in Foot Shape: The development of bunions, hammertoes, or Charcot foot (a collapse of the foot’s arch due to neuropathy).
Perform a Daily Foot Check: This is non-negotiable. Inspect the tops, sides, soles, heels, and between every toe every single day. Use a mirror if needed or ask a family member for help. You’re looking for anything new or different.
The Essential 8-Point Prevention Plan

Prevention is your most powerful tool. Integrate these strategies into your daily life:
1. Master Blood Sugar Control.
This is the foundation. Keeping your blood glucose within your target range helps slow the progression of neuropathy and PAD, and boosts your immune response. Work closely with your healthcare team on medication, diet, and exercise.
2. Conduct the Daily Foot Inspection.
As described above. Make it a habit like brushing your teeth.
3. Wash and Moisturize Daily.
· Wash feet in lukewarm (not hot) water. Test temperature with your elbow.
· Dry thoroughly, especially between toes.
· Apply a thin layer of moisturizer (like urea-based cream) on dry areas, but not between toes, as excess moisture there can lead to fungal infection.
4. Wear Appropriate Footwear at All Times.
· Never walk barefoot, even indoors.
· Wear well-fitted, supportive shoes with a wide toe box. Break new shoes in slowly.
· Consider prescription diabetic shoes and custom orthotic inserts if recommended.
· Always check inside your shoes for debris or rough spots with your hand before putting them on.

5. Trim Nails Safely.
· Cut nails straight across, not curved at the edges.
· File sharp edges with an emery board.
· If you have thickened nails, poor vision, or neuropathy, have a podiatrist (foot doctor) trim them.
6. Protect Feet from Temperature Extremes.
· Avoid heating pads, hot water bottles, or soaking feet in hot water.
· Wear socks in cold weather.
7. Stay Active to Promote Circulation.
Engage in foot-safe activities like walking, swimming, or cycling, as approved by your doctor. Move your ankles and wiggle your toes periodically throughout the day.
8. Schedule Regular Professional Foot Care.
See a podiatrist or healthcare provider specializing in diabetic foot care at least once a year (more often if you have any risk factors like a history of ulcers, neuropathy, or PAD). They can perform a comprehensive foot exam, manage calluses, and provide expert guidance.
What to Do If You Find a Problem: The “When to Call” Rule
If you notice any of the following, contact your doctor or podiatrist the same day:
· A cut, blister, sore, ulcer, or bruise that does not begin to heal in 48 hours.
· Any area of redness, swelling, or warmth.
· An ingrown toenail or a corn/callus with bleeding.
· Pain in your legs or feet, even at rest.
Go to the Emergency Room immediately if you see:

· A deep, infected, or foul-smelling wound.
· Blackened tissue (gangrene).
· A fever or chills in combination with a foot wound.
A Final Note of Empowerment
Managing diabetic foot health requires diligence, but it is a profound act of self-care. By understanding the risks, committing to daily inspection, and partnering with your healthcare team, you take powerful control over your health. Your feet carry you through life—give them the careful attention they deserve.
FAQs
Basics & Causes

1. What exactly is a diabetic foot ulcer?
Answer: A diabetic foot ulcer (DFU) is an open sore or wound that typically occurs on the bottom of the foot in people with diabetes. It’s more than a simple cut—it’s a complex wound that develops due to a combination of nerve damage (neuropathy), poor circulation, and high blood sugar, which together prevent normal healing and increase infection risk.
2. Why are people with diabetes so prone to foot ulcers?
Answer: Three main factors create a “perfect storm”:
· Neuropathy: High blood sugar damages nerves, causing loss of sensation. You might not feel a blister or cut.
· Poor Circulation: Diabetes narrows blood vessels, reducing blood flow to the feet. Less blood means less oxygen and nutrients for healing.
· Immune Impairment: High glucose weakens white blood cells, making it harder to fight infection in a wound.
3. I have diabetes but feel fine. Could I still be at risk?
Answer: Yes, absolutely. Nerve damage (neuropathy) often develops gradually and without pain. You can have significant nerve damage and reduced circulation while still “feeling fine.” Regular foot exams by a professional are essential, as they can detect problems before you feel them.
Early Signs & Detection
4. What are the very first signs I should watch for?
Answer: Before an ulcer forms, watch for:
· Skin changes: Redness, warmth, or coolness; dry, cracked skin (especially heels); thick calluses.
· Color changes: Pale, blue, or darkened skin.
· Swelling in the foot or ankle.
· New pain (aching, cramping) or a tingling/burning sensation.
· Any change in the shape of your foot (like a new bunion or collapsed arch).
5. How do I perform a proper daily foot check?

Answer:
1. When: Do it at the same time daily (e.g., after bathing).
2. Where: Use a well-lit room.
3. Method: Check the tops, bottoms, sides, heels, and between every toe. Use a hand mirror for the soles or ask a family member for help.
4. What: Look for ANYTHING new—cuts, blisters, redness, swelling, discoloration, or broken skin.
6. Is a callus or corn something to worry about?
Answer: Yes. Calluses and corns form from repeated pressure (often due to ill-fitting shoes or foot deformities). They can become thick and ulcerate underneath. Never cut them yourself or use over-the-counter acid patches. Have them assessed and safely managed by a podiatrist.
Prevention Strategies

7. What are the most important things I can do to prevent ulcers?
Answer: The “Big Three” are:
1. Control Your Blood Sugar: This is the foundation for slowing nerve and blood vessel damage.
2. Inspect Your Feet Daily: Never miss a day.
3. Wear Proper Footwear: Always wear shoes, even indoors. Choose well-fitting, supportive shoes with a wide toe box. Break new shoes in slowly.
8. What type of shoes should I wear?
Answer: Look for:
· Deep toe box to prevent rubbing.
· Soft, seamless interior to minimize friction.
· Firm heel counter for support.
· Adjustable closure (laces or Velcro).
Consider prescription diabetic shoes if you have significant neuropathy, deformities, or a history of ulcers. These are custom-fitted to redistribute pressure.

9. Can I soak my feet to keep them clean?
Answer: No. Do not soak your feet. Soaking dries out the skin, leading to cracks, and you risk burning yourself if you have neuropathy and can’t feel the water temperature. Wash feet daily with lukewarm water and mild soap, pat them dry thoroughly (especially between toes), and apply moisturizer (but not between toes).
10. How should I trim my toenails?
Answer:
· Cut straight across, never curved at the corners.
· File sharp edges with a nail file.
· If you have neuropathy, poor vision, or thickened nails: Have a podiatrist or healthcare professional trim them. The risk of a self-inflicted cut is too high.
Treatment & Emergency Care
11. What should I do if I find a small cut or blister?
Answer:
1. Clean it gently with saline or mild soap and water.
2. Apply an antibiotic ointment.
3. Cover it with a sterile, non-stick bandage (like a Telfa pad).
4. Keep pressure off it. Don’t walk on that area.
5. Contact your doctor or podiatrist immediately—even for minor wounds. Don’t adopt a “wait and see” approach.
12. When is a foot ulcer a medical emergency? Go to the ER if you see:
· Fever or chills.
· Red streaks running up your leg from the wound.
· Increased pain, redness, swelling, or warmth.
· Pus or foul-smelling drainage.
· Blackened tissue (gangrene).
· New numbness or an inability to move the foot.
13. Why is “off-loading” so important for healing an ulcer?
Answer: Off-loading means removing all pressure from the ulcer site. Continuing to walk on an ulcer destroys new healing tissue and grinds the wound deeper. Doctors use special boots (like a total contact cast), crutches, or specialized shoes to ensure the area gets complete rest. This is the single most important part of treatment besides infection control.
Lifestyle & Professional Care

14. How often should I see a foot doctor (podiatrist)?
Answer:
· Low Risk (no neuropathy or PAD): At least once a year for a comprehensive foot exam.
· High Risk (has neuropathy, poor circulation, foot deformity, or history of ulcer): Every 2-3 months, or as directed by your healthcare team.
15. Does smoking really affect my feet?
Answer: Yes, critically. Smoking dramatically accelerates peripheral arterial disease (PAD) by narrowing your blood vessels even further. It severely reduces the blood flow your feet need to heal. Quitting smoking is one of the most powerful things you can do for your foot health.