When you get a cut, scrape, or surgical incision, your body doesn’t just patch the hole—it orchestrates a sophisticated, multi-stage rebuilding project. At the heart of this project lies a remarkable protein: collagen. Often mentioned in skincare ads and supplement aisles, collagen’s true biological role is far more profound than reducing wrinkles. It is the essential architectural framework, the literal scaffolding of your skin, and its production is the cornerstone of wound healing.
The Blueprint: Understanding the “Healing Cascade”
To appreciate collagen’s role, we need to understand the four stages of wound healing, where collagen is the star of the third act:
1. Hemostasis (Stop the Bleeding): Platelets form a clot.
2. Inflammation (Clean the Site): Immune cells clear debris and bacteria.
3. Proliferation (Rebuild the Tissue): This is collagen’s moment. New tissue, rich in collagen, fills the wound.
4. Remodeling (Strengthen the Scar): Collagen fibers reorganize and mature over months or years.
Act III: The Proliferation Phase – Where Collagen Takes Center Stage
Once the wound is clean, your body shifts from demolition to construction. Special cells called fibroblasts migrate into the wound bed. Think of them as the master builders, and their primary building material is Type III collagen.
· The Construction Site: The wound bed becomes a hive of activity. Fibroblasts begin synthesizing and secreting strands of collagen, along with other proteins like elastin.
· Building the Scaffold: These collagen strands are laid down in a haphazard, criss-crossing mesh. This mesh, called granulation tissue, is what gives a healthy healing wound its characteristic pink, bumpy appearance. It’s fragile but vital—it fills the defect and creates a base for new skin cells to crawl across.
· The Cover-Up: Simultaneously, epithelial cells (skin cells) at the wound edges multiply and migrate over this new collagen scaffold, eventually meeting in the middle to form a new surface layer.
From Fragile Mesh to Strong Scaffold: The Maturation Phase
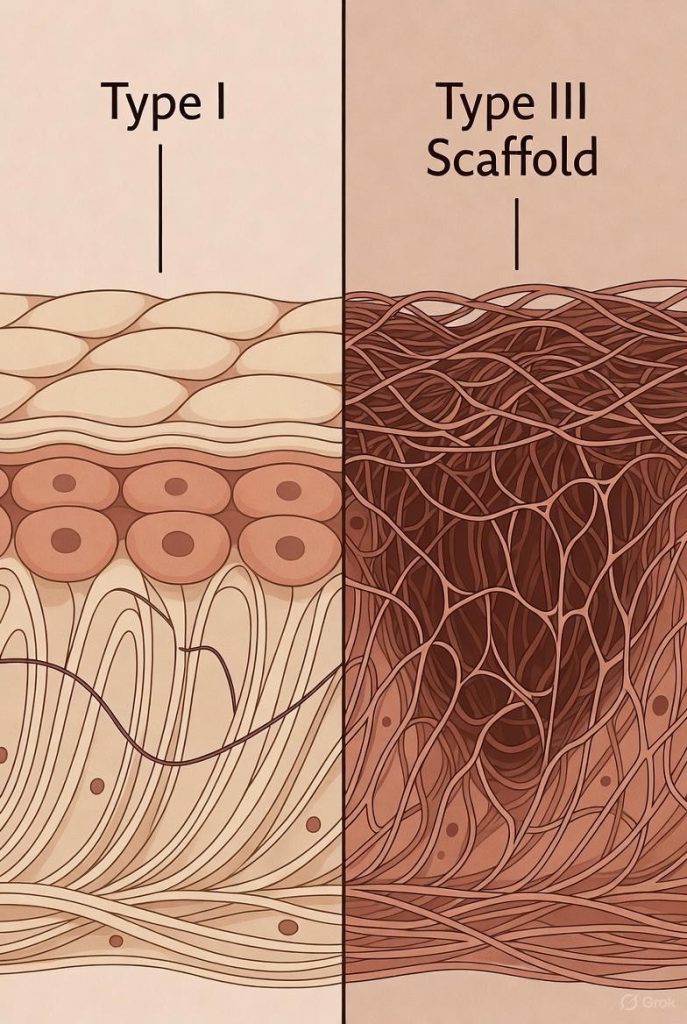
The initial collagen laid down (Type III) is fine and quick to produce, but it’s not very strong. If healing stopped here, the skin would tear easily. Enter the final, longest phase: Remodeling.
Over the next 3 to 24 months, your body meticulously remodels the wound:
· Fiber Reorganization: Fibroblasts, now acting like contractors, realign the chaotic collagen mesh. They break down the initial Type III collagen and replace it with stronger, more organized Type I collagen (the main type found in healthy skin).
· Cross-Linking for Strength: Enzymes create chemical bonds (cross-links) between collagen fibers, dramatically increasing tensile strength. Remarkably, a fully healed scar will regain about 80% of the original skin’s strength.
· The Scar Matures: This process of breaking down and rebuilding is why scars change over time—from red and raised to paler, flatter, and softer.
What Supports (and Sabotages) Collagen Production?
Your body needs specific raw materials and conditions to build collagen effectively.
Supporting Your Body’s Builders:
· Vitamin C: The absolute essential. Without it, fibroblasts cannot synthesize collagen. This is why scurvy (severe Vit C deficiency) causes old wounds to re-open.
· Protein: Collagen is a protein. Adequate dietary protein (from meat, fish, eggs, legumes) provides the necessary amino acids, like glycine and proline.
· Zinc & Copper: Cofactors for the enzymes that build and cross-link collagen fibers.
· A Clean, Moist Wound Environment: Research shows a moist wound bed supports optimal fibroblast activity and collagen deposition better than a dry, scabbed one.
Common Saboteurs:
· Poor Blood Sugar Control: High glucose levels can stiffen and tangle collagen fibers (a process called glycation), impairing proper formation.
· Smoking: Nicotine constricts blood vessels, starving fibroblasts of oxygen and nutrients. It also introduces thousands of toxins that disrupt the building process.
· Chronic Stress: Elevates cortisol, a hormone that breaks down collagen.
· Infection: Prolongs the destructive inflammatory phase and diverts resources away from rebuilding.
Collagen Supplements and Topical Creams: Do They Help Healing?
This is a complex question:
· Oral Supplements: When digested, collagen is broken into amino acids. There is emerging evidence that specific collagen peptides may stimulate your own fibroblasts, but the science is not yet definitive for acute wound healing. They are not a substitute for the nutritional building blocks from a whole-food diet.
· Topical Creams: Most collagen molecules are too large to penetrate the skin’s barrier. While they can provide moisturizing benefits, they do not directly become part of your new skin’s scaffold. Prescription silicone gels or sheets are more clinically proven to influence scar appearance by improving collagen organization during remodeling.
The Bottom Line: Respect the Process
Collagen is not just a trendy ingredient; it is the fundamental structural protein your body uses to literally knit itself back together. A healing wound is a monumental feat of biological engineering, with fibroblasts working tirelessly to weave a new matrix of strength and resilience.
You can support this incredible innate process by providing the right nutrients, protecting the wound, and avoiding the saboteurs. By understanding collagen’s crucial role, we gain a deeper appreciation for the complex, intelligent healing happening beneath the bandage—and learn how to be better allies to our own bodies on the path to recovery.
FAQs
Q1: Is the collagen my body produces the same as what’s in supplements?
Answer: Structurally, yes—both are made from the same amino acids. However, supplemental collagen is not a “plug-and-play” building block. When you ingest collagen supplements, your digestive system breaks them down into individual amino acids and small peptides. These components are then absorbed and may stimulate your own fibroblasts to produce more collagen, but they don’t get directly woven into your wound as-is. Your body still controls the construction process.
Q2: Will taking collagen supplements make my wound heal faster?
Answer: The evidence is promising but not definitive. Some clinical studies show that specific collagen peptides can support skin elasticity and hydration, and may enhance healing in certain contexts (like pressure ulcers). However, for typical acute wounds in otherwise healthy individuals, ensuring adequate overall protein and Vitamin C intake is likely just as critical. Supplements should complement, not replace, a nutrient-rich diet.
Q3: What’s the difference between Type I, Type II, and Type III collagen mentioned in healing?
Answer:
· Type I: The “mature” and strongest collagen. It’s the main component of healthy skin, tendons, and bones. During remodeling, it replaces Type III to strengthen the scar.
· Type II: Found primarily in cartilage. It’s not a major player in skin wound healing.
· Type III: The “quick-fix” collagen. It’s finer and more flexible, laid down rapidly during the proliferation phase to form the initial scaffold (granulation tissue). It’s later replaced by Type I.
Q4: Why do some scars become thick, raised, or discolored (like keloids)?
Answer: This is often a result of disordered collagen production and remodeling. In conditions like keloids or hypertrophic scars, fibroblasts become overactive and produce too much collagen, or the collagen fibers fail to reorganize properly during maturation. Genetics, wound location (e.g., chest, shoulders), and prolonged inflammation all contribute to this abnormal collagen architecture.
Q5: If a moist environment is best, should I avoid letting a wound “scab” or “air out”?
Answer: Yes, the modern medical consensus favors moist wound healing over air-drying. A scab is the body’s natural bandage, but it can trap bacteria underneath and creates a physical barrier that skin cells must crawl under, slowing healing. Using a simple occlusive or hydrocolloid bandage maintains a clean, moist environment that supports fibroblast activity and collagen deposition, often leading to faster healing with less scarring.
Q6: How long does it take for collagen to fully rebuild after a deep cut or surgery?
Answer: The timeline has two parts:
1. Initial Deposition (Proliferation): Fibroblasts begin laying down new collagen within 3-5 days, filling the wound over the next few weeks.
2. Remodeling & Strengthening (Maturation): This phase is lengthy. Collagen reorganization and strengthening begin around 3 weeks post-injury and continue for 12-24 months. While the wound may look closed in weeks, the underlying collagen is still maturing for up to two years.
Q7: Can you rebuild collagen in old scars?
Answer: To a limited extent, yes. While you cannot completely remodel an old scar, you can improve its appearance and pliability. Methods include:
· Medical Treatments: Laser therapy, microneedling, and silicone sheets can stimulate controlled collagen remodeling in the scar tissue.
· Topical Products: Prescription retinoids (like tretinoin) can promote collagen production in the surrounding skin.
· Massage: Regular scar massage during the maturation phase (first 6-24 months) can help align collagen fibers and break up adhesions.
Q8: Does age really affect collagen production in healing?
Answer: Yes, significantly. As we age, fibroblast activity slows, and the balance of collagen production shifts. Older adults produce less overall collagen and more of the fragile Type III relative to strong Type I. This results in generally slower healing and skin that is more prone to tearing. This is why supporting nutrition and wound care is especially critical for older individuals.
Q9: Are there signs my wound isn’t producing enough collagen?
Answer: Yes, watch for signs of a chronic or stalled wound:
· The wound bed appears pale, smooth, and shiny (like hard plastic), lacking the pink, bumpy “granulation tissue.”
· The wound fails to decrease in size or depth over several weeks.
· The edges are hardened and rolled under (epibole).
These are signs to seek evaluation from a wound care specialist.
Q10: Beyond Vitamin C, what foods directly support collagen synthesis?
Answer: Focus on a “Collagen-Builder’s Plate”:
· Protein Sources: Chicken, fish (especially with skin), bone broth, eggs, beans (provide amino acids).
· Co-Factor Foods: Citrus fruits & bell peppers (Vitamin C), oysters & pumpkin seeds (zinc), nuts & seeds (copper), dark leafy greens (antioxidants).
· Avoid: Excess sugar and processed carbs, which can promote inflammation and collagen damage (glycation).
Key Takeaway:
Your body is an expert builder, and collagen is its most vital construction material for healing. You can’t outsource the work entirely to a supplement, but you can be an exceptional foreman by providing the right raw materials (nutrition), a safe worksite (clean, moist wound care), and eliminating saboteurs (like smoking). Trust the process, support it intelligently, and respect the months-long journey from initial repair to final, resilient strength.