When we hear the word “depression,” many of us picture someone feeling persistently sad, hopeless, and losing interest in things they once loved. While this classic picture is accurate for Major Depressive Disorder, the world of depressive illnesses is far more nuanced.
Depression doesn’t always look the same for everyone. It can wear different masks, manifest in unexpected ways, and be tied to specific life circumstances or biological functions. Understanding these variations is crucial for empathy, reducing stigma, and ensuring people get the right kind of help.
Here are five types of depression you might not be familiar with.
1. Persistent Depressive Disorder (PDD) – The Slow Burn

Formerly known as Dysthymia, Persistent Depressive Disorder is a chronic form of depression where a low, dark, or sad mood is present more often than not for at least two years (one year for children and adolescents).
· What it feels like: Think of it not as a sudden downpour, but as a constant, drizzling rain that colors your entire life. People with PDD often describe feeling as if they’ve “always been this way.” They can usually function in their daily lives—going to work, maintaining relationships—but they operate under a heavy cloud of gloom, low energy, and poor self-esteem. It’s the “slow burn” of depression.
· Why it’s often missed: Because the symptoms are less acute and have been present for so long, individuals may dismiss it as just part of their personality—being “pessimistic” or a “worrier.”
2. Seasonal Affective Disorder (SAD) – The Winter Fog

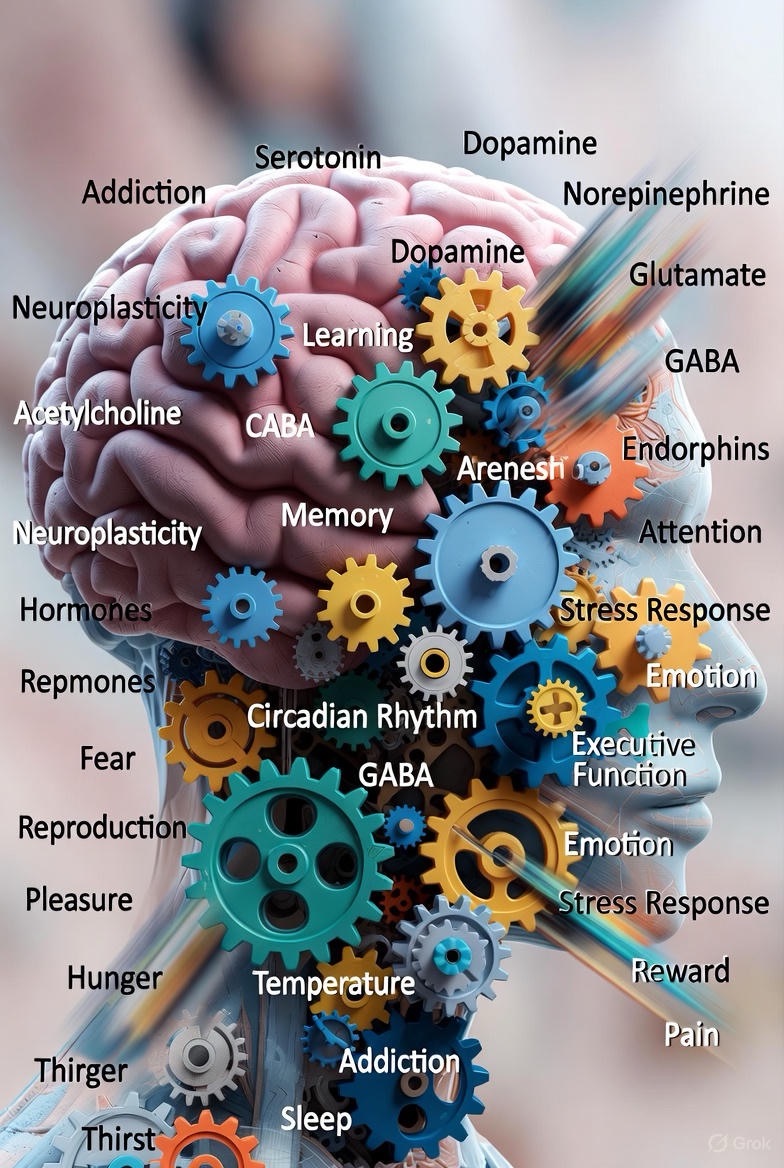
This one is more than just the “winter blues.” Seasonal Affective Disorder is a type of depression that follows a strict seasonal pattern, most commonly beginning in the late fall or early winter and easing during the spring and summer.
· What it feels like: It’s like a mental and physical hibernation. Symptoms often include overwhelming fatigue, increased need for sleep, cravings for carbohydrates, and weight gain. It’s as if your body and brain are slowing down in response to the shorter days and reduced sunlight.
· Why it’s often missed: People might blame themselves for feeling lazy or unmotivated during the winter months, not realizing there’s a biological basis tied to disruptions in your circadian rhythm and serotonin levels.
3. Peripartum (Postpartum) Depression – More Than “Baby Blues”

While most people have heard of postpartum depression, many don’t realize its full scope. The term “Peripartum Depression” is now used because it can actually start during pregnancy, not just after. It’s a profound mood disorder that goes far beyond the typical “baby blues,” which are mild and short-lived.
· What it feels like: It’s an intense mix of overwhelming sadness, anxiety, and exhaustion that makes it difficult for a new or expecting parent to care for themselves or their baby. It can be accompanied by terrifying thoughts, a sense of detachment from the baby, and intense guilt about not feeling the “joy” they’re supposed to feel.
· Why it’s often missed: The immense social pressure to be a “happy new parent” can lead to shame and silence. Symptoms are often dismissed as normal stress or sleep deprivation, preventing many from seeking the critical help they need.
4. Situational Depression – The Overwhelmed Spirit
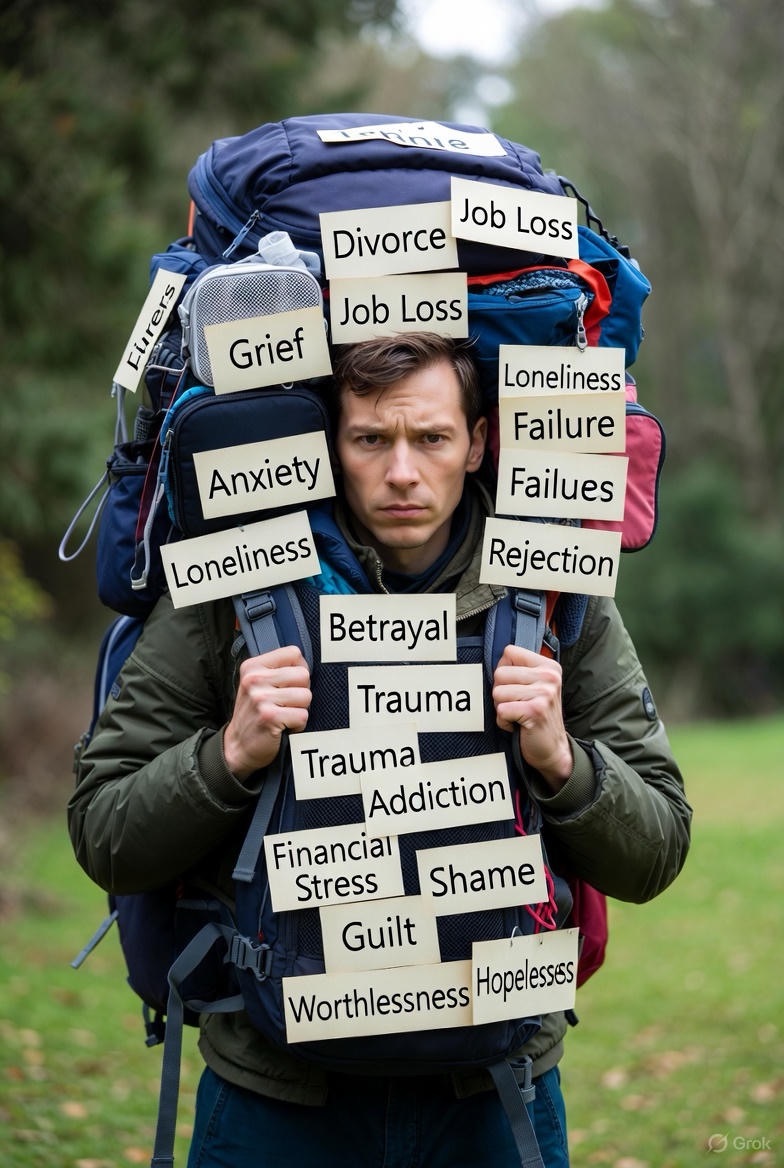
Clinically known as Adjustment Disorder with Depressed Mood, this type is triggered by a specific, stressful life event. This could be a divorce, job loss, the death of a loved one, a serious diagnosis, or any major life change.
· What it feels like: It’s a feeling of being completely overwhelmed and unable to cope. The emotional and behavioral symptoms—intense sadness, worry, and feeling unable to manage daily tasks—are a direct reaction to the external stressor.
· Why it’s often missed: Well-meaning people might say, “It’s normal to feel this way given what you’re going through.” While true, when these feelings become debilitating and persist beyond a typical adjustment period, it crosses into a clinical territory that benefits from professional support.
5. Atypical Depression – The Depression That Flips the Script
This subtype is ironically named “atypical” because it is actually quite common. What makes it different are its unique features that seem to contradict classic depression.
· What it feels like: The key characteristic is mood reactivity. This means your mood can temporarily brighten in response to positive events (like a friend visiting or receiving good news). Other hallmark symptoms include:
· Increased appetite or weight gain (instead of loss).
· Heavy, leaden feelings in the arms and legs.
· Sleeping excessively (hypersomnia).
· Why it’s often missed: Because the person can seem “fine” or even cheerful at times, their struggle may be minimized. Their symptoms, like overeating and oversleeping, can be mistaken for laziness or a lack of discipline rather than signs of a biological illness.
The Most Important Takeaway: You Are Not Alone

If you see yourself in any of these descriptions, the most vital step is to reach out. These are real, valid, and treatable medical conditions—not character flaws or personal weaknesses.
Understanding the different faces of depression helps us break down the harmful “one-size-fits-all” stereotype. It empowers us to recognize our own struggles or those of a loved one with more clarity and compassion.
Your journey matters. Your feelings are valid. And help is available.
If you need to talk to someone, you can reach out to:
· The 988 Suicide & Crisis Lifeline: Call or text 988 (in the US and Canada).
· Crisis Text Line: Text HOME to 741741.
· The National Alliance on Mental Illness (NAMI): 1-800-950-NAMI (6264) or www.nami.org
FAQs
1. How is clinical depression different from just feeling sad or stressed?
Answer: Normal sadness or stress is typically a temporary reaction to a specific event and doesn’t consistently interfere with your ability to function. Clinical depression is a medical condition characterized by persistent symptoms (like changes in sleep, appetite, energy, and concentration) that last for at least two weeks and significantly impact your daily life. It’s not a sign of weakness, and it often doesn’t have a single, clear cause.
2. Can I have more than one of these types of depression at the same time?
Answer: Yes, this is possible and is known as comorbidity. For example, a person with Persistent Depressive Disorder (PDD) can also experience a major depressive episode on top of it (“double depression”). Similarly, someone with Seasonal Affective Disorder (SAD) might go through a traumatic event and develop Situational Depression during a difficult season.

3. What’s the difference between Situational Depression and Major Depression?
Answer: The key difference is the cause and duration.
· Situational Depression (Adjustment Disorder) is a direct, intense reaction to a specific, identifiable stressor (e.g., a divorce, job loss). It typically lessens as the person adapts or the situation improves.
· Major Depression can appear without an obvious external trigger and involves a more severe set of symptoms that persist consistently for at least two weeks. The cause is often a complex mix of genetic, biological, environmental, and psychological factors.
4. I think I might have one of these. How do I get a formal diagnosis?
Answer: The best first step is to schedule an appointment with a healthcare professional who can perform an assessment. This could be:
· Your primary care doctor (to rule out any underlying medical conditions).
· A psychiatrist (a medical doctor who can diagnose and prescribe medication).
· A psychologist or licensed therapist (who can provide a diagnosis and therapy).
They will conduct a clinical interview, asking about your thoughts, feelings, symptoms, and medical history to make an accurate diagnosis.

5. For Atypical Depression, if my mood can improve, does that mean I’m not really depressed?
Answer: No, not at all. This is the defining feature of “mood reactivity” in Atypical Depression. The ability to feel temporary relief or happiness in response to positive events does not invalidate your struggle. The core symptoms of depression (like leaden paralysis, overeating, and hypersomnia) are still present and debilitating. It’s the pattern of symptoms that defines this subtype.
6. Are the treatments for these different types of depression unique?
Answer: While core treatments like psychotherapy (especially CBT) and antidepressant medication are effective for many forms of depression, the approach is often tailored.
· SAD is frequently treated with light therapy in addition to traditional methods.
· Situational Depression often responds very well to short-term, focused therapy that builds coping skills.
· Peripartum Depression requires a approach that considers the safety of both parent and baby, often involving specialists in maternal mental health.
A professional will create a treatment plan based on your specific diagnosis and needs.
7. How can I explain this to my family or friends who don’t understand?
Answer: It can be helpful to use analogies. You could say:
· “It’s not just sadness. It’s more like a broken arm you can’t see; I need treatment to heal.”
· “My brain chemistry is affecting my energy and mood, just like diabetes affects blood sugar. It’s a medical condition.”
You can also share reputable articles (like this one) to help them understand that depression has many forms.
8. If I have Persistent Depressive Disorder, have I just been “like this” my whole life? Is it too late for treatment?
Answer: It is never too late for treatment. Many people with PDD have spent so long feeling this way that they believe it’s an unchangeable part of their personality. However, PDD is highly treatable. Therapy can provide new coping mechanisms, and medication can help correct underlying neurochemical issues, allowing you to experience a level of wellness you may not have thought possible.
9. What can I do to help myself, in addition to professional treatment?

Answer: Self-care is a valuable support to professional treatment. While not a cure, these practices can help manage symptoms:
· Routine: Try to stick to a daily schedule, even when you don’t feel like it.
· Movement: Gentle exercise, like a daily walk, can boost mood.
· Nutrition: Eat balanced meals to support your body and brain.
· Sleep Hygiene: Aim for consistent sleep and wake times.
· Mindfulness: Practices like meditation or deep breathing can reduce anxiety.
Be patient with yourself and celebrate small victories.
10. Is Peripartum Depression the same as postpartum anxiety or psychosis?
Answer: No, they are related but distinct conditions.
· Peripartum Depression involves profound sadness, hopelessness, and fatigue.
· Postpartum Anxiety often involves intense, uncontrollable worry, racing thoughts, and physical symptoms of panic.
· Postpartum Psychosis is a rare but severe medical emergency characterized by hallucinations, delusions, and confusion. It requires immediate medical attention.
All are serious conditions that deserve compassionate, professional care.

