We all get cuts, scrapes, and burns from time to time. Most heal within days or weeks, a testament to the body’s remarkable ability to repair itself. But sometimes, a wound lingers, refusing to close, becoming a source of pain, frustration, and significant health risk. This difference—between a wound that heals and one that stalls—boils down to a critical distinction: acute versus chronic.
Understanding this difference isn’t just medical jargon; it’s key to getting the right care, preventing complications, and supporting your body’s healing journey.

The Basics: The Healing Cascade
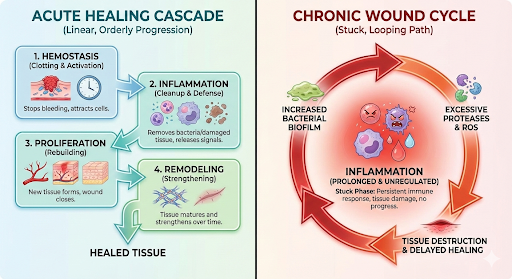
To grasp the acute vs. chronic divide, it helps to know the normal healing process. Your body repairs an acute wound in four orderly, overlapping stages:
1. Hemostasis: The immediate response. Blood vessels constrict and a clot forms to stop bleeding.
2. Inflammation: The cleanup crew arrives. Blood flow increases, bringing white blood cells to fight infection and remove debris. This causes redness, warmth, and swelling.
3. Proliferation: The rebuild phase. New tissue (granulation tissue) fills the wound, new blood vessels form, and skin cells (epithelial cells) begin to migrate across the surface.
4. Maturation/Remodeling: The finishing touches. The new tissue gains strength and flexibility as collagen fibers reorganize. This final phase can last for months or years, with the scar gradually fading.
Acute Wounds: The Predictable Path to Recovery

An acute wound is a recent injury that progresses predictably and orderly through the four stages of healing within an expected timeframe—typically less than 4 weeks.
Examples:
· Surgical incisions
· Simple lacerations (cuts)
· Abrasions (scrapes)
· First- and second-degree burns
· Minor puncture wounds
Key Characteristics:
· Clear Cause: Has a specific, identifiable onset (e.g., a fall, a knife cut).
· Predictable Timeline: Follows the standard healing stages without significant delay.
· Healthy Wound Bed: Appears pink or red, may be moist, and shows visible signs of shrinkage and new tissue growth.
· Response to Standard Care: Typically heals well with basic first aid: cleaning, protection from infection, and keeping it moist with a simple bandage.
Chronic Wounds: The Stalled Healing Process

A wound is classified as chronic when it fails to progress through the normal, orderly stages of healing within 4 to 6 weeks. It gets “stuck,” most commonly in the inflammatory phase, creating a cycle of ongoing tissue damage and failed repair.
Examples:
· Pressure Injuries (Bedsores): From prolonged pressure on skin, often over bony areas.
· Diabetic Foot Ulcers: A devastating complication of diabetes, often on the sole of the foot.
· Venous Leg Ulcers: Caused by poor circulation in the leg veins, usually around the ankle.
· Arterial Ulcers: Caused by poor arterial blood flow, often on the feet or toes.
· Non-healing surgical wounds.
Key Characteristics:
· Underlying Health Cause: Often rooted in a systemic condition (diabetes, vascular disease, immobility).
· Prolonged Inflammation: The wound appears stuck—persistently red, swollen, painful, and may have excess drainage.
· No Visible Progress: Shows no signs of shrinkage or new tissue growth over weeks.
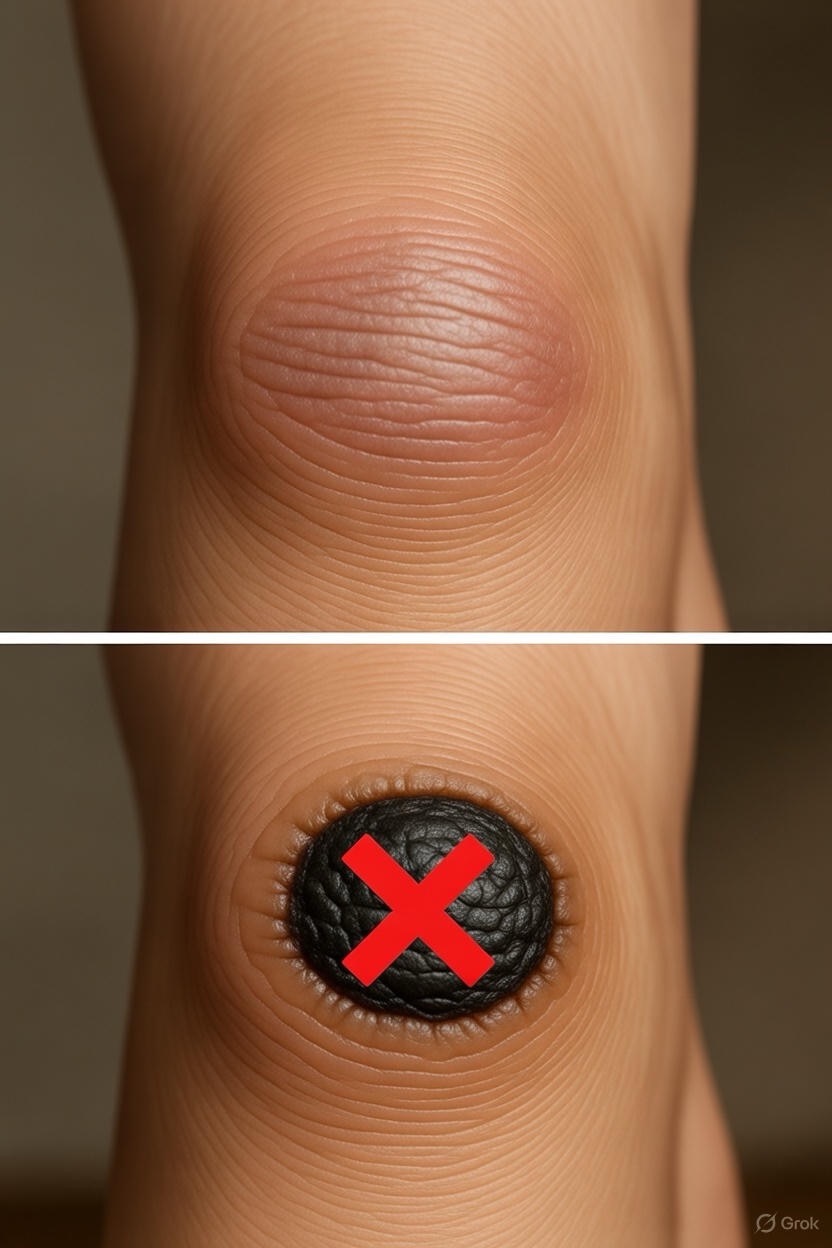
· Atypical Appearance: May have a yellow or black necrotic tissue (slough or eschar), pale or dark wound bed, or rolled edges.
· Requires Specialized Care: Will not heal with basic first aid alone.
Why the Difference Matters Profoundly

1. Treatment Approach is Radically Different:
· Acute Wound Care: Focuses on infection prevention and supporting the body’s innate process.
· Chronic Wound Care: Requires a multidisciplinary approach. Treatment must address the underlying cause (e.g., off-loading pressure for a diabetic ulcer, compression therapy for a venous ulcer) in addition to advanced wound dressings, debridement (removal of dead tissue), and sometimes advanced therapies like negative pressure wound therapy.
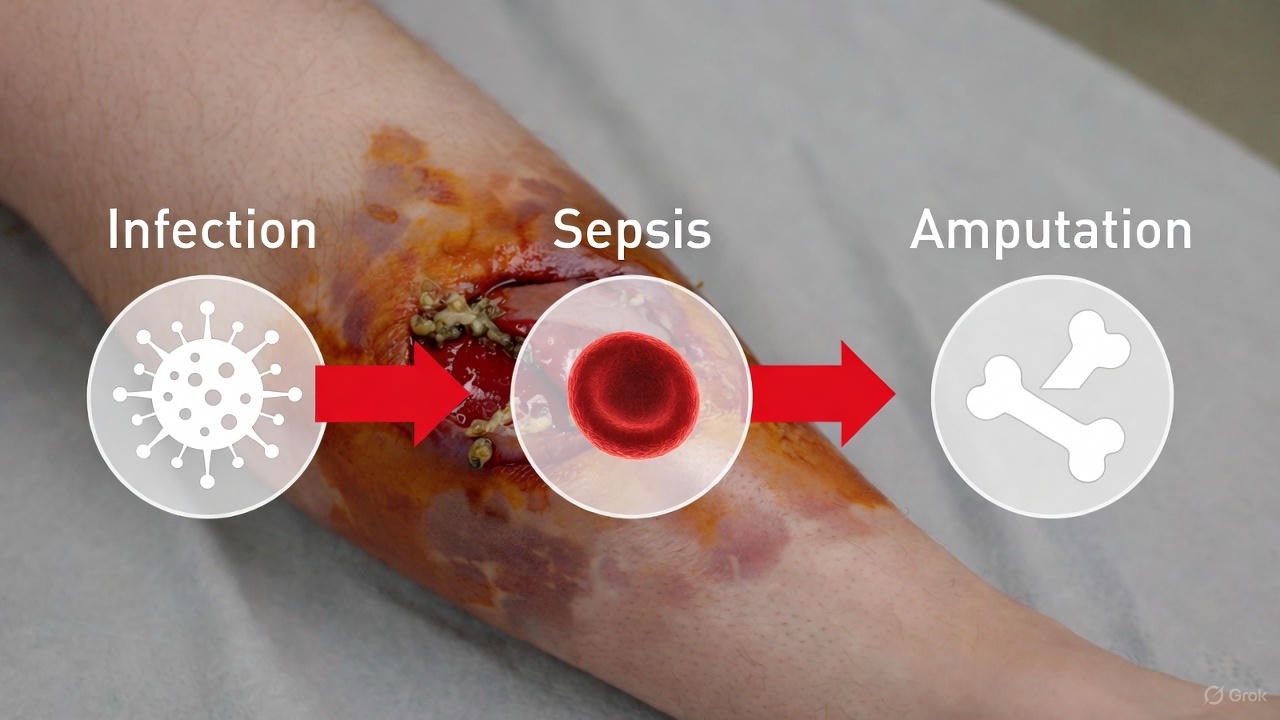
2. Risk of Complications Skyrockets:
Chronic wounds are a portal for serious infection, including cellulitis, bone infections (osteomyelitis), and sepsis. The longer a wound remains open, the higher the risk.
3. Impact on Quality of Life:
Chronic wounds can be debilitating, causing chronic pain, foul odor, significant mobility limitations, social isolation, and depression. They represent a major burden for patients and the healthcare system.
4. It’s a Warning Sign:
A chronic wound is rarely an isolated problem. It is a visible signal of an underlying health issue that must be diagnosed and managed. A diabetic foot ulcer is a direct warning about blood sugar control and vascular health.
When to Seek Professional Help: Red Flags

Don’t wait 6 weeks to act. See a doctor or a wound care specialist if a wound shows any of these signs:
· Shows no improvement in size or appearance after 2 weeks.
· Is increasingly red, swollen, warm, or painful (signs of infection).
· Has spreading redness from the wound site.
· Produces pus or excessive drainage.
· Develops a foul odor.
· Is accompanied by fever or chills.
· Is associated with diabetes, poor circulation, or immobility.
The Bottom Line: Mindset Matters
Think of an acute wound as a simple repair job and a chronic wound as a complex construction project with broken equipment. The latter requires an expert project manager (your healthcare team), specialized tools (advanced dressings and therapies), and fixing the underlying equipment failure (the systemic health condition).
If you or a loved one has a wound that isn’t healing, the most important step is to seek specialized care. Wound care centers specialize in diagnosing the cause of the stall and creating a targeted treatment plan. Remember, time is tissue. Prompt, appropriate care is the key to closing the chapter on a chronic wound and restoring health and mobility.

FAQs
Q1: What’s the simplest way to tell if a wound is acute or chronic?
Answer: Time and progress. An acute wound shows steady, visible improvement (shrinking, less redness, new pink tissue) and is largely or fully healed within 3-4 weeks. A chronic wound shows little to no progress in healing for 4-6 weeks or more, often staying the same size or even worsening despite basic care. If a wound isn’t getting better after two weeks of proper care, it’s time to see a doctor.
Q2: Can an acute wound become chronic?
Answer: Yes, absolutely. An acute wound can transition to chronic if:
· An underlying health condition (like undiagnosed diabetes or vascular disease) impairs healing.
· It becomes infected and the infection is not properly treated.
· There is ongoing pressure, friction, or trauma to the area (e.g., continuing to walk on a diabetic foot blister).
· Poor nutrition, smoking, or certain medications (like steroids) delay the healing process.

Q3: Why do chronic wounds get “stuck” in the inflammation stage?
Answer: Think of inflammation as the body’s cleanup and alarm phase. In chronic wounds, the initial cause of damage (like pressure or poor blood flow) often persists, constantly re-injuring the tissue. This creates a cycle where the body keeps sounding the alarm (inflammation) but can’t move on to the repair and rebuild phases. High levels of destructive enzymes and bacteria in the wound can also perpetuate this stalled state.
Q4: Are chronic wounds always painful?
Answer: Not always, and the lack of pain can be dangerously misleading.
· Venous ulcers may be only mildly painful but are often itchy and swollen.
· Diabetic foot ulcers are frequently painless due to underlying nerve damage (neuropathy). This is why people with diabetes must do daily visual foot checks.
· Arterial ulcers and pressure injuries are often very painful.
The level of pain is not a reliable indicator of severity.
Q5: Is a wound with a scab healing or becoming chronic?
Answer: A scab (eschar) is the body’s natural “biological bandage” for acute, superficial wounds. However, a dark, hard, leathery black scab on a deep or large wound can be a sign of necrosis (dead tissue). This type of eschar acts as a barrier to healing and must often be removed by a medical professional (debridement) for a chronic wound to heal. If in doubt, have a healthcare provider assess it.
Q6: I have diabetes. Why are my wounds at higher risk of becoming chronic?
Answer: Diabetes can impair healing through a “perfect storm” of effects:
1. Neuropathy: Nerve damage reduces sensation, so injuries go unnoticed and untreated.
2. Poor Circulation: Reduced blood flow limits the delivery of oxygen and nutrients needed for repair.
3. Immune Dysfunction: High blood sugar weakens white blood cells, raising infection risk.
4. Cellular Dysfunction: The cells involved in building new tissue don’t function properly.
This is why proactive foot care and immediate attention to any skin break is critical for people with diabetes.
Q7: What’s the most important thing I can do to prevent a wound from becoming chronic?
Answer: Address the underlying cause immediately and maintain meticulous wound hygiene.
· For pressure injuries: Relieve pressure through frequent repositioning and proper support surfaces.
· For diabetic foot ulcers: See a podiatrist, wear appropriate footwear, and off-load pressure from the wound site.
· For venous leg ulcers: Use compression therapy as prescribed.
· For all wounds: Keep the wound clean and appropriately moist (not wet or dry), protect it from further trauma, and ensure excellent nutrition (especially adequate protein, vitamin C, and zinc).
Q8: Do I need to see a specialist for a chronic wound?
Answer: Yes, it is highly recommended. While your primary care doctor can start the process, a wound care specialist or a dedicated Wound Care Center has expertise in advanced dressings, debridement techniques, and therapies (like negative pressure wound therapy) that are essential for healing complex, stalled wounds. They also lead a team that may include vascular surgeons, podiatrists, and infectious disease doctors.
Q9: How does nutrition affect wound healing?

Answer: Profoundly. The body needs extra energy and specific building blocks to repair tissue.
· Protein: The fundamental building block for new skin and tissue.
· Vitamin C: Essential for forming collagen, the structural protein of skin.
· Zinc: Aids in cell growth and immune function.
· Vitamin A: Supports epithelial cell growth and immune response.
Malnutrition or poor intake can single-handedly turn an acute wound into a chronic one.
Q10: What are the dangers of an untreated chronic wound?
Answer: The risks escalate from local to systemic, including:
1. Serious Infection: Cellulitis (skin infection), abscess, and osteomyelitis (bone infection).
2. Sepsis: A life-threatening body-wide response to infection.
3. Amputation: Particularly in cases of non-healing diabetic foot ulcers or severe arterial disease.
4. Squamous Cell Carcinoma: Rarely, a long-standing chronic wound can develop into skin cancer (Marjolin’s Ulcer).
This is why early, aggressive treatment is crucial.
Key Takeaway:
The shift from acute to chronic is a critical tipping point. Time is tissue. The most powerful actions you can take are recognizing a stalled wound early and seeking specialized care to address both the wound itself and the underlying health problem causing the stall. Your body wants to heal; sometimes it needs the right expert help to get back on track.