The decision to start therapy is a powerful act of self-care. Yet, for many, the path from that decision to the first session can feel shrouded in mystery, fueled by questions, and sometimes, held back by stigma. If you’re wondering, “Where do I even begin?” you’re not alone.
This guide is your roadmap. Let’s replace the confusion with clarity and the apprehension with action. Seeking support isn’t a sign of weakness; it’s a sign of strength and a commitment to your own well-being.
Step 1: Understanding the “Why” – It’s More Than “Being Fix”

Therapy isn’t just for crises. People start therapy to:
· Navigate life transitions (career change, loss, relationships)
· Understand and manage emotions like anxiety, sadness, or anger
· Break unhelpful patterns in behavior or thinking
· Heal from past trauma
· Simply have a dedicated, unbiased space for self-exploration and growth
Think of it less like going to a mechanic to “get fixed” and more like hiring a personal trainer for your mental and emotional fitness.
Step 2: The Different “Gyms” – Common Types of Therapy

Just as there are different workout styles, there are different therapeutic approaches. A therapist often blends these, but knowing the terms helps you find a good fit.
· Cognitive Behavioral Therapy (CBT): The most widely practiced. Focuses on identifying and changing unhelpful thought and behavior patterns in the present. Highly structured and goal-oriented. Great for anxiety, depression, and phobias.
· Psychodynamic Therapy: Explores how past experiences, often from childhood, shape your current feelings and behaviors. Focuses on self-awareness and understanding deep-seated patterns.
· Humanistic Therapy (Person-Centered): Centers on your innate capacity for growth. The therapist provides a supportive, non-judgmental environment for you to find your own solutions. Less directive, more reflective.
· Acceptance and Commitment Therapy (ACT): Teaches mindfulness and acceptance skills to handle difficult thoughts and feelings, while committing to actions aligned with your personal values.
· Dialectical Behavior Therapy (DBT): A form of CBT that emphasizes coping skills for managing intense emotions, improving relationships, and mindfulness. Particularly effective for emotional dysregulation.
· Couples or Family Therapy: Focuses on improving communication and dynamics within relationships, not on any one individual.
Step 3: The “Trainers” – Who’s Who in Mental Health Care

· Psychologist (Ph.D. or Psy.D.): Holds a doctorate and provides therapy and psychological testing. Cannot prescribe medication (except in a few states with additional training).
· Licensed Clinical Social Worker (LCSW): Trained in therapy and case management, often with a strengths-based, systems-oriented approach.
· Licensed Professional Counselor (LPC) / Licensed Mental Health Counselor (LMHC): Master’s-level clinicians trained specifically in counseling techniques.
· Marriage and Family Therapist (LMFT): Specializes in relationship and family dynamics.
· Psychiatrist (M.D.): A medical doctor who can diagnose, prescribe medication, and sometimes provide therapy. Often focuses on medication management.
For most people starting talk therapy, a psychologist, LCSW, LPC, or LMFT is an excellent starting point.
Step 4: The Practical Hunt – How to Find a Therapist

1. Use Your Insurance: Go to your insurer’s website and use their “Find a Provider” tool. Filter by specialty (e.g., “anxiety,” “trauma”) and location.
2. Use a Reputable Directory:
· Psychology Today: The largest directory. You can filter by location, insurance, specialty, and approach. Robust profiles with photos and introductory videos.
· TherapyDen: Includes filters for inclusivity (LGBTQ+ affirming, social justice-oriented, etc.).
· Open Path Collective: A nonprofit for affordable therapy ($40-70/session) if you’re uninsured or underinsured.
3. Ask for Referrals: Trusted friends, your primary care physician, or a local university’s counseling center can often provide names.
Step 5: The First Date – What to Expect in Your First Session
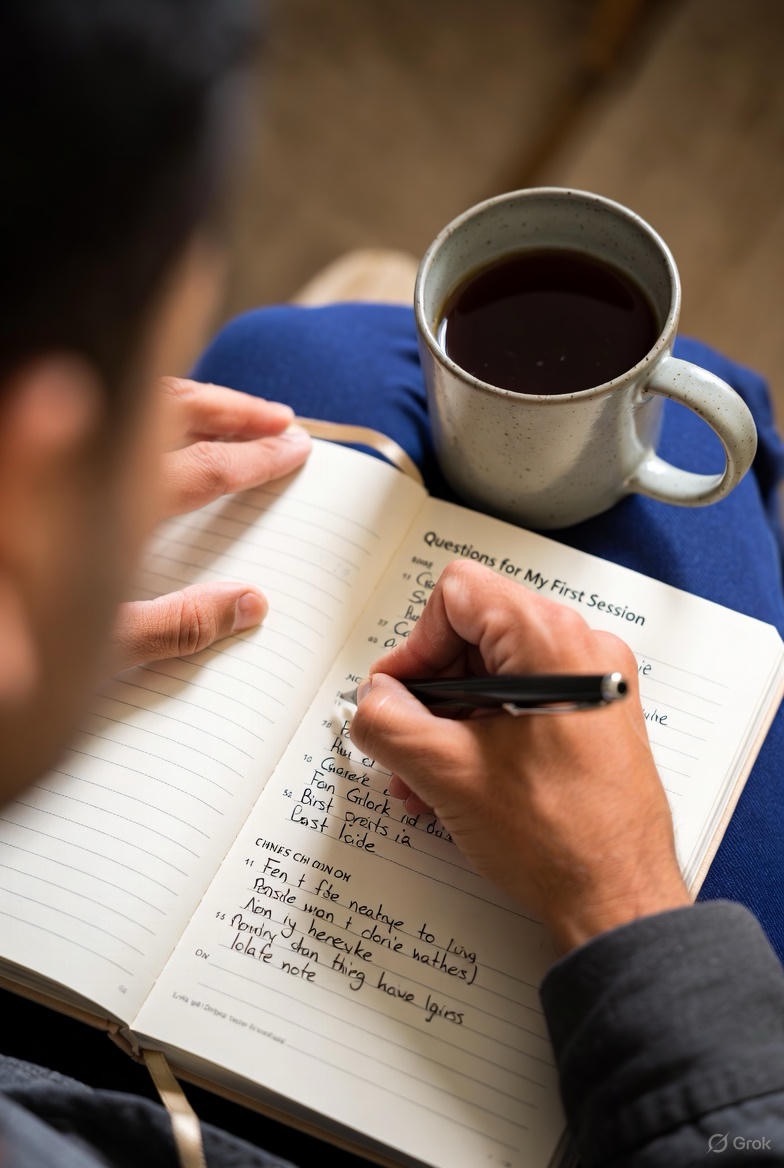
The initial session is a mutual interview. Your goal is to see if you feel safe and understood. Their goal is to understand your needs.
· You’ll likely be asked: “What brings you in?” “What are you hoping to achieve?” You don’t need a perfect answer; “I’ve been feeling overwhelmed and want to understand why” is enough.
· You should ask: “What is your experience with [my concern]?” “What is your approach?” “How do we know if therapy is working?”
· You’ll discuss logistics: Fees, insurance, cancellation policies, and session frequency (usually weekly at first).
· Pay attention to fit: Do you feel heard? Comfortable? This “therapeutic alliance” is the strongest predictor of success. It’s okay to try a few therapists to find the right match.
Step 6: Navigating the Hurdles – Common Concerns

· “It’s too expensive.” Many therapists offer sliding scale fees. Check community mental health centers and training clinics (where supervised interns offer low-cost care).
· “I don’t have time.” Many therapists offer evening/weekend slots. Telehealth (video therapy) has also made access easier.
· “What if I don’t know what to say?” Your therapist is trained to guide the conversation. Silence is okay. You can even start by saying, “I’m not sure what to say.”
· Stigma: Remember, you are prioritizing your health. The narrative is changing; this is a modern, proactive step millions take.
Starting therapy is a brave and hopeful beginning. It’s a space that is entirely yours—to be honest, to be messy, to be curious, and ultimately, to heal and grow. Take the first step of searching for a provider today. Your future self will thank you.
Need immediate help? You are not alone. If you are in crisis or having thoughts of harm, call or text the 988 Suicide & Crisis Lifeline for free, confidential support 24/7.
FAQs
Q1: How do I know if I really need therapy or if I should just handle things on my own?
A: This is a very common question. Therapy is not just for “severe” problems. Consider it if:
· Your usual coping methods aren’t working.
· Your feelings or thoughts are impacting your work, relationships, or daily functioning.
· You feel stuck in patterns you can’t break.
· You want objective, professional guidance for personal growth.
You don’t need to be in crisis to benefit—think of it as preventative care for your mind.

Q2: What’s the difference between a therapist, psychologist, and psychiatrist?
A:
· Therapist/Counselor: An umbrella term for licensed professionals (LCSW, LPC, LMFT) who provide talk therapy.
· Psychologist: Has a PhD or PsyD, provides therapy and psychological testing, but typically cannot prescribe medication.
· Psychiatrist: A medical doctor (MD or DO) who can prescribe medication and sometimes provide therapy, but often focuses on medication management.
For most people starting talk therapy, a therapist or psychologist is the right first step.
Q3: How do I find a therapist who takes my insurance?
A: The most direct way is to:
1. Check your insurance company’s website for their “Find a Provider” directory.
2. Filter by “behavioral health” or “mental health.”
3. Call the therapist’s office directly to verify they are currently accepting your specific plan.
You can also use directories like PsychologyToday.com and filter by your insurance provider.

Q4: What if I can’t afford therapy?
A: There are options:
· Sliding Scale: Many therapists adjust fees based on your income. Always ask.
· Community Health Centers: Offer low-cost mental health services.
· Training Clinics: University psychology departments often have clinics where supervised graduate students provide low-cost therapy.
· Open Path Collective: A nonprofit offering sessions between $40-$70.
· Online Platforms: Some like BetterHelp or Talkspace can be more affordable, but research their privacy policies.
Q5: What should I ask a potential therapist in a first call?
A:
· “Do you have experience helping people with [my specific concern]?”
· “What is your therapeutic approach?”
· “What are your fees, and do you offer a sliding scale?”
· “What is your availability?”
· “How do you typically measure progress?”
Their answers—and how comfortable you feel talking to them—will help you decide.
Q6: What actually happens in the first session?
A: The first session (often called an “intake”) is primarily an assessment. You’ll discuss:
· What brought you to therapy.
· Your personal history and current life.
· Your goals for treatment.
· Logistics like confidentiality, fees, and scheduling.
It’s a chance for you both to see if you’re a good fit. You don’t have to share your deepest secret right away.
Q7: How long does therapy take?
A: There’s no one-size-fits-all answer. Some people benefit from short-term, goal-oriented therapy (8-12 sessions), while others engage in longer-term work for deeper exploration. You and your therapist will regularly check in on progress and discuss the timeline.

Q8: How do I know if a therapist is a good fit for me?
A: Pay attention to how you feel. A good fit often means you feel:
· Heard, respected, and understood.
· Comfortable being honest, even when it’s difficult.
· Collaboratively engaged in the process.
It’s okay to try 2-3 sessions to gauge the fit. It’s also perfectly acceptable to try another therapist if it doesn’t feel right—this is a critical part of the process.
Q9: Is everything I say really confidential?
A: Yes, with very specific, legally mandated exceptions that your therapist must explain to you (this is “informed consent”). These exceptions typically include:
· Immediate risk of harm to yourself or others.
· Suspected abuse or neglect of a child, elder, or dependent adult.
· A court order.
Your privacy is a cornerstone of therapy.
Q10: What if I start feeling worse?
A: Sometimes, bringing up difficult emotions can initially feel more intense. This is often a normal part of the process as you begin to process things you’ve avoided. It’s crucial to tell your therapist this. They can help you navigate these feelings and adjust the pace. If the feeling is extreme or doesn’t shift, it may be a sign to discuss a different approach.

Q11: Can I do therapy online? Is it effective?
A: Yes, telehealth (video therapy) is a widely accepted and effective option. Research shows it can be just as effective as in-person therapy for many conditions. It offers greater accessibility and convenience. The most important factor remains the quality of the therapeutic relationship, regardless of the format.
Q12: How do I end therapy when I’m ready?
A: Ideally, you and your therapist will recognize your progress together and plan for a final session or a “tapering off” period. This allows for closure, a review of what you’ve learned, and a discussion of a maintenance plan. You have the right to end therapy at any time, but it’s most beneficial to have a final session to process the ending.

