Imagine you’re at home and accidentally scrape your knee, or you’re caring for a loved one with a surgical incision. The first question that often comes to mind is: What kind of bandage should I use? Walk down the first-aid aisle of any pharmacy and you’ll find an overwhelming array of options—gauze pads, adhesive films, hydrogel sheets, foam dressings, and more. Choosing the right wound dressing isn’t just about covering the wound; it’s about creating the optimal environment for healing.
Modern wound care has evolved far beyond the simple gauze-and-tape approach. The right dressing can speed up recovery, reduce pain, lower infection risk, and even minimize scarring. Here’s a guide to help you navigate the world of wound dressings and pick the best one for your situation.
Understanding the Goal: Moist Wound Healing
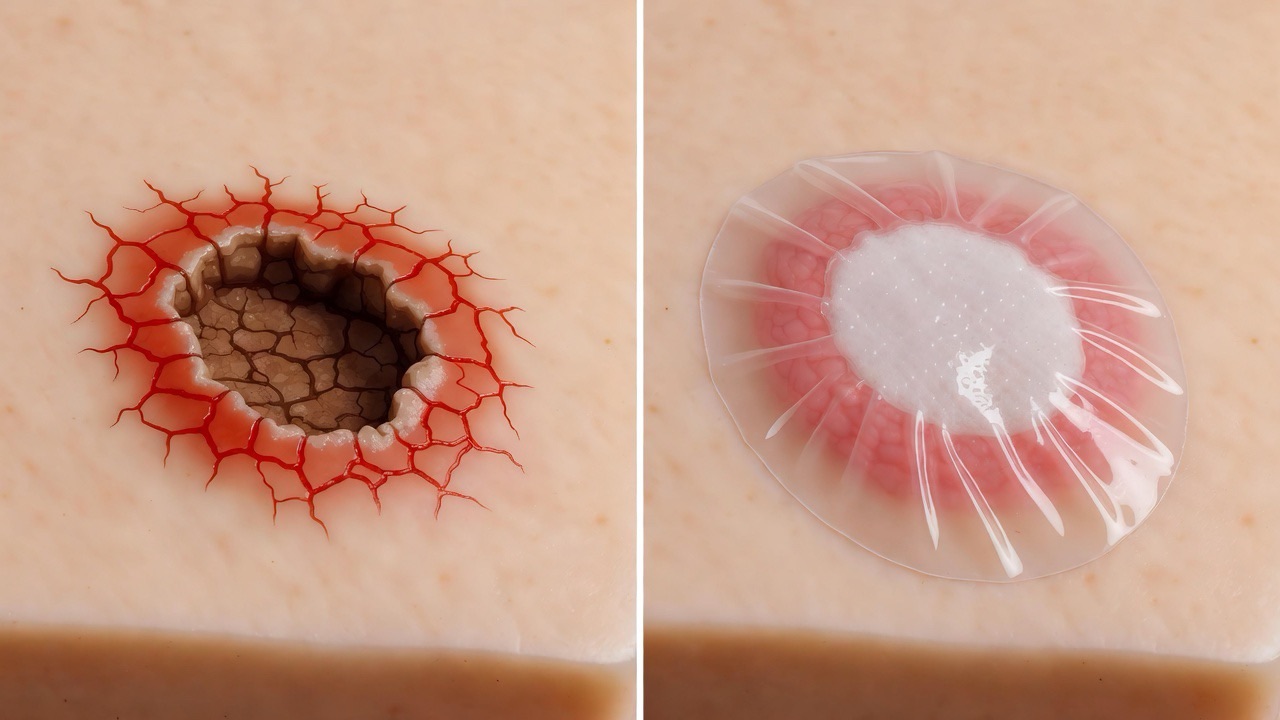
For decades, the common belief was that wounds should be kept dry and exposed to air. Science has since proven that moist wound healing is far more effective. A moist environment helps cells move more easily to repair tissue, reduces scab formation (which can slow healing), and often decreases pain. The key is choosing a dressing that maintains this ideal moisture balance—neither too wet nor too dry.
Common Types of Wound Dressings
1. Gauze Dressings
· What they are: Traditional woven or non-woven cotton pads, often used with medical tape or as part of a kit.
· Best for: Large, heavily draining wounds; cleaning wounds; secondary dressings (over another primary dressing).
· Pros: Inexpensive, highly absorbent, readily available.
· Cons: Can stick to the wound bed (causing pain upon removal), may leave fibers behind, requires frequent changes, and can dry out the wound if not monitored.
· Tip: If using gauze on an open wound, consider a non-adherent variety or moisten it with sterile saline before removal.
2. Transparent Film Dressings
· What they are: Thin, adhesive, see-through sheets (like Tegaderm™).
· Best for: Protecting intact or nearly healed skin; IV sites; superficial wounds with minimal drainage.
· Pros: Waterproof, allow easy wound monitoring without removal, maintain a moist environment.
· Cons: Not absorbent; can trap excess moisture leading to maceration (softening) of surrounding skin.

3. Hydrocolloid Dressings
· What they are: Flexible, wafer-like dressings that contain gel-forming agents (like pectin or gelatin).
· Best for: Light to moderately draining wounds; blisters, pressure sores, or partial-thickness wounds.
· Pros: Provide a moist healing environment, are waterproof, can be left on for several days, and are painless to remove.
· Cons: Not for infected wounds or heavy drainage; may leave a slight odor upon removal (this is normal).
4. Hydrogel Dressings
· What they are: Water- or glycerin-based gels, available in sheets or amorphous gel form.
· Best for: Dry or necrotic wounds; painful wounds; burns; providing soothing hydration.
· Pros: Cool and soothe, rehydrate dry wound beds, reduce pain, and are non-adherent.
· Cons: Require a secondary dressing to hold in place; not for wounds with heavy exudate.
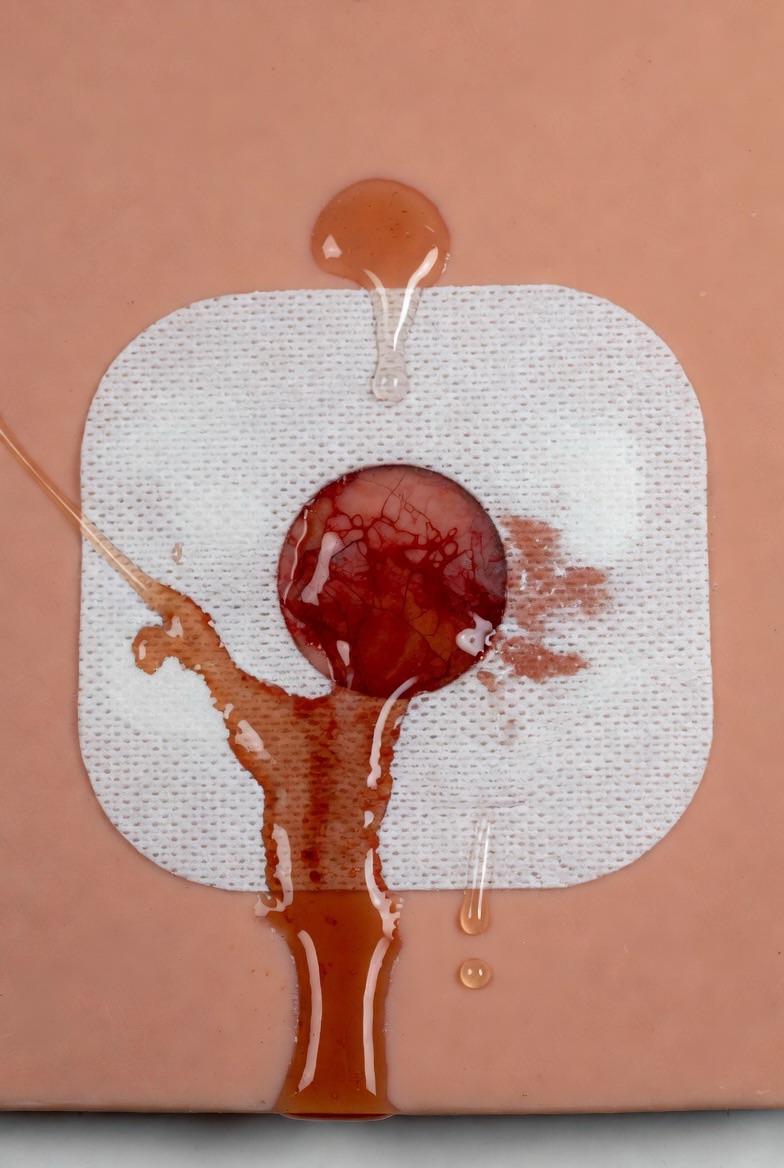
5. Foam Dressings
· What they are: Soft, absorbent pads made from polyurethane foam.
· Best for: Moderate to heavy drainage; sensitive skin; under compression bandages.
· Pros: Highly absorbent, cushion and protect, maintain a moist environment, and are easy to remove.
· Cons: May require a secondary dressing; not for dry wounds or wounds with no drainage.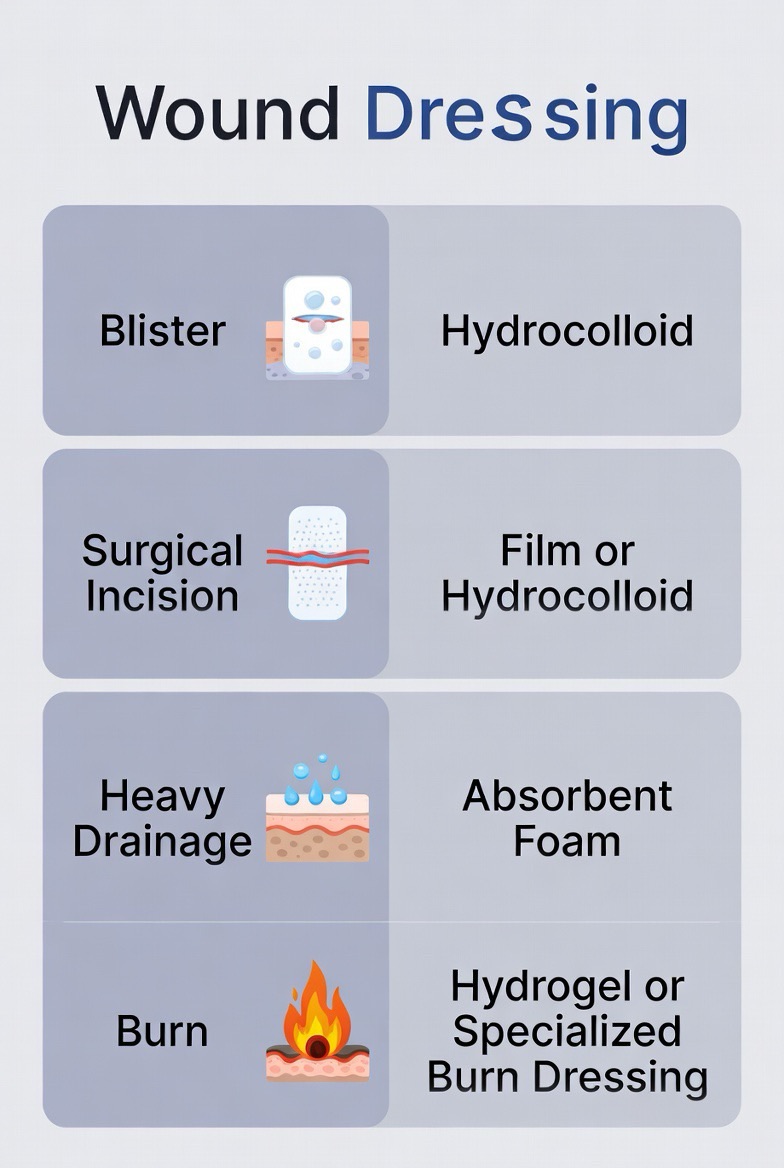
6. Alginate Dressings
· What they are: Highly absorbent dressings derived from seaweed, usually in rope or pad form.
· Best for: Heavy to very heavy draining wounds; bleeding wounds (they help with clotting).
· Pros: Excellent absorption, conform to wound shape, and are biodegradable.
· Cons: Require a secondary dressing; not for dry wounds or third-degree burns.
7. Antimicrobial Dressings
· What they are: Dressings impregnated with agents like silver, iodine, or honey to reduce bacteria.
· Best for: Wounds at risk of infection, or mildly infected wounds (under medical guidance).
· Pros: Help control infection locally, can reduce odor.
· Cons: Should not be used long-term without supervision; can be more expensive.
Choosing the Right Dressing: A Quick-Reference Chart
Wound Type Recommended Dressing Why
Minor cuts/scrapes Film or hydrocolloid Protects, maintains moisture, allows monitoring.
Blisters Hydrocolloid Cushions, prevents further friction, speeds healing.
Heavy drainage (e.g., ulcer) Foam or alginate Manages exudate, protects surrounding skin.
Dry, sloughy, or necrotic wound Hydrogel Rehydrates tissue to support autolytic debridement.
Surgical incision (closed) Film or silicone mesh Protects, minimizes scarring, reduces friction.
Burn (superficial) Hydrogel or specialty film Cools, soothes, provides moisture.
At-risk of infection Antimicrobial (e.g., silver) Reduces bacterial load.
When to See a Doctor
While many minor wounds can be managed at home, seek medical attention if:
· The wound is deep, gaping, or won’t stop bleeding.
· Signs of infection appear (increased redness, warmth, swelling, pus, or fever).
· The wound involves a puncture or animal/human bite.
· There’s a foreign object embedded.
· You have an underlying condition like diabetes or poor circulation.

Final Thoughts
Selecting the right wound dressing is a small but powerful step in the healing journey. By matching the dressing to the wound’s needs—considering drainage, depth, and stage of healing—you support your body’s natural repair processes more effectively.
Remember, this guide is for informational purposes. For chronic or complex wounds, always consult a healthcare professional for a tailored treatment plan. Here’s to faster, more comfortable healing with the simple power of the right bandage!
FAQs
1. What’s wrong with just using a regular bandage or gauze and tape?
Regular gauze and adhesive bandages are fine for minor, everyday cuts. However, if a wound is larger, has more drainage, or is slow-healing, traditional gauze can stick to the wound bed (causing pain and damage during changes) and may create a dry environment that slows healing. Modern dressings are designed to maintain moist wound healing, which is clinically proven to speed recovery and reduce scarring.
2. How often should I change my wound dressing?
It depends entirely on the dressing type and the wound:
· Hydrocolloids, films, and some foams: Can often stay on for 3–7 days, unless they’re leaking or the wound smells/turns red.
· Gauze on a draining wound: May need changing 1–2 times daily.
· General rule: Change it if the dressing is soaked through, loose, dirty, or if you notice signs of infection. Always follow your healthcare provider’s instructions or the product’s guidelines.
3. Is it better to let a wound “air out” or keep it covered?
Keep it covered. Letting a wound dry out and form a hard scab actually slows healing and increases scarring. A moist, covered environment helps skin cells migrate and repair faster. Covering also protects from bacteria and further injury.
4. What dressing should I use for a wound that’s leaking a lot of fluid?
For heavy drainage, use a highly absorbent dressing like:
· Foam dressings
· Alginate dressings (for very heavy exudate)
· Specialty superabsorbent pads
These pull moisture away from the wound bed and protect the surrounding skin from becoming soggy and broken down (maceration).
5. What if the dressing sticks to my wound?
This is common with gauze or dried-out dressings. To prevent it:
· Use a non-adherent or silicone-based dressing designed not to stick.
· If using gauze, choose a non-stick variety or moisten it with sterile saline or water before gently lifting it off.
· Never rip it off dry—soak it first to avoid reopening the wound.

6. Can I get my dressing wet in the shower?
It depends:
· Waterproof dressings (films, hydrocolloids, some foams): Yes, but avoid direct high-pressure water jets.
· Non-waterproof dressings (gauze, many absorptive pads): No. Cover them with a waterproof barrier (like a plastic wrap sealed with tape) or use a specialized waterproof cover.
· When in doubt, keep it dry and consider a sponge bath for the area.
7. What does it mean if my wound smells bad under the dressing?
A faint, sweet, or chemical smell can be normal with some dressings like hydrocolloids as they interact with wound fluid. However, a foul, rotten, or strong odor can indicate infection or necrotic tissue. If it’s accompanied by increased pain, redness, or pus, see a doctor.
8. What should I use for a sensitive skin or if I’m allergic to adhesives?
Look for:
· Hypoallergenic paper or silicone tape
· Soft silicone dressings (these adhere gently to dry skin but not the wound itself)
· Non-adherent pads secured with a stretch gauze wrap or tubular netting
· Avoid latex and strong adhesives if you have known sensitivities.
9. How do I know if a wound is infected?
Signs of infection include:
· Increasing redness, warmth, or swelling spreading from the wound
· Thick yellow, green, or foul-smelling pus
· Increased or throbbing pain
· Fever or chills
If you suspect infection, seek medical attention. Do not just change the dressing—you may need antibiotics.
10. Are antimicrobial (silver/honey) dressings better for healing?
Not always. They are excellent for wounds at high risk of infection or with signs of early infection, as they help reduce bacterial load. However, for clean, low-risk wounds, a standard moist dressing is often sufficient and more cost-effective. Overuse of antimicrobials can sometimes irritate skin or slow healing in non-infected wounds.
11. What’s the best dressing for a burn?
· Minor first-degree burns (red, no blisters): Aloe vera gel and a non-stick dressing or a hydrogel sheet to cool and soothe.
· Second-degree burns (blisters, raw skin): Do not pop blisters. Use a specialized burn dressing, hydrogel, or silicone-coated dressing that won’t stick. See a doctor for larger burns.
· Never use cotton balls or fluffy dressings that can stick to burns.
12. Can I use the same dressing for the entire healing process?
Probably not. As a wound heals, its needs change:
· Heavy drainage phase: Use an absorbent dressing (foam/alginate).
· As drainage slows: Switch to a less absorbent option (hydrocolloid/thin foam).
· Final healing/scar management: A silicone sheet or film may be used to protect and minimize scarring.
Reassess the wound each time you change the dressing.
13. Where can I buy these specialized dressings?
· Basic types (films, hydrocolloids, foam): Available at most pharmacies, large retailers, or online.
· Medical-grade or advanced types (alginate, silver, silicone): Often at medical supply stores, pharmacies with large wound-care sections, or online retailers. Some may require a prescription for insurance coverage.
14. When should I definitely see a doctor instead of self-treating?
· The wound is deep, gaping, or won’t stop bleeding with pressure.
· It’s a puncture wound or from a dirty/rusty object (tetanus risk).
· There are signs of infection (as above).
· You have diabetes, poor circulation, or a compromised immune system.
· The wound isn’t improving after 1–2 weeks of proper care.

