It starts with a racing heart, a sense of dread, thoughts spinning like a carousel you can’t get off. This is anxiety.
Then, it shifts. The energy drains away, leaving a heavy blanket of numbness, a void where joy used to be. This is depression.
If you’ve experienced both, you’re far from alone. While they feel like opposites—one a state of frantic “too much,” the other a state of hollow “not enough”—depression and anxiety are intimately connected. In fact, it’s estimated that nearly half of all people diagnosed with depression also struggle with an anxiety disorder.
So, why do they so often hold hands? And what does it mean when you live with this challenging duo? Let’s untangle the threads of the anxious heart.

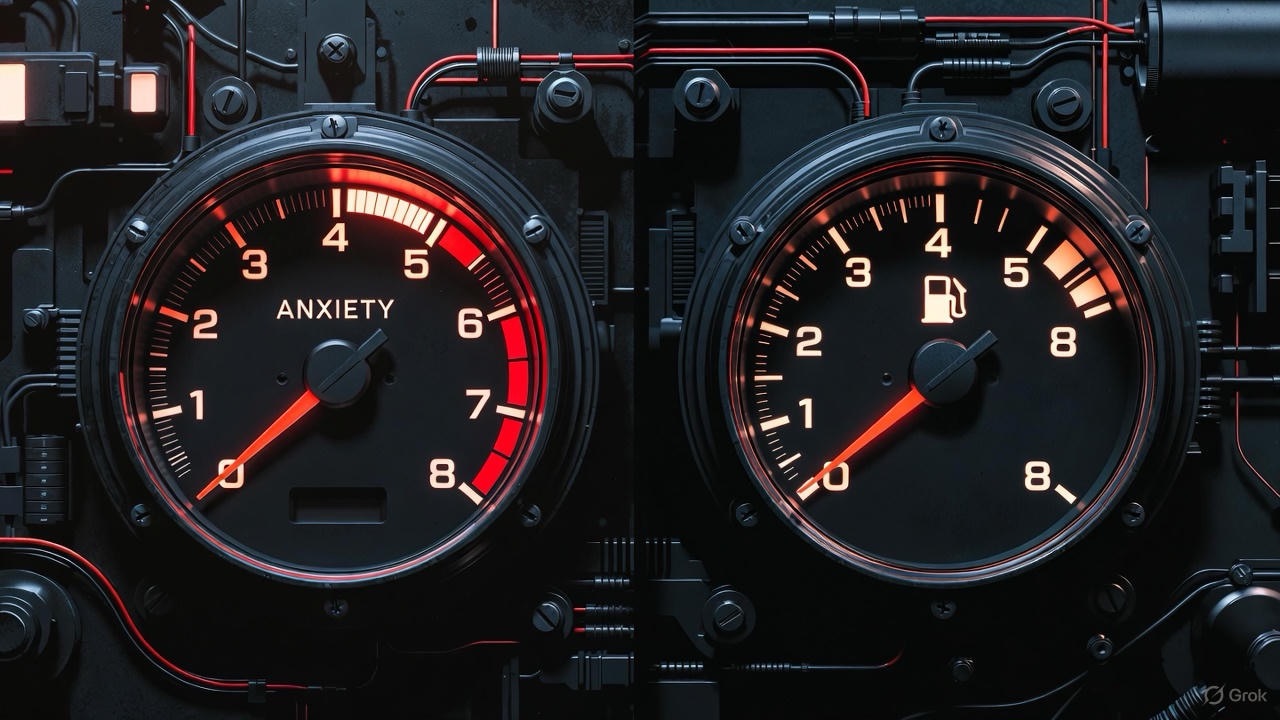
The Vicious Cycle: How Anxiety and Depression Fuel Each Other
Imagine anxiety as a relentless alarm system. It’s constantly on high alert, scanning for threats and shouting, “Something bad is going to happen!” This state of hypervigilance is exhausting. The constant worry, the physical tension, the inability to relax—it drains your mental and physical batteries.
Over time, this exhaustion can become a gateway to depression. You may start to feel hopeless, believing you’ll never escape the cycle of worry. You might withdraw from activities and social connections because they feel too overwhelming. This isolation and loss of pleasure are classic hallmarks of depression.
Now, flip the perspective. Depression brings profound fatigue, low self-esteem, and a sense of despair. When you’re in this state, your ability to cope with life’s normal stresses plummets. A small problem can feel insurmountable. This feeling of being overwhelmed and unable to cope then triggers… anxiety.
This creates a self-perpetuating loop:
Anxiety -> Exhaustion & Avoidance -> Depression -> Poor Coping & Overwhelm -> Anxiety
It’s not a straight line; it’s a tangled knot where one thread inevitably pulls the other tighter.
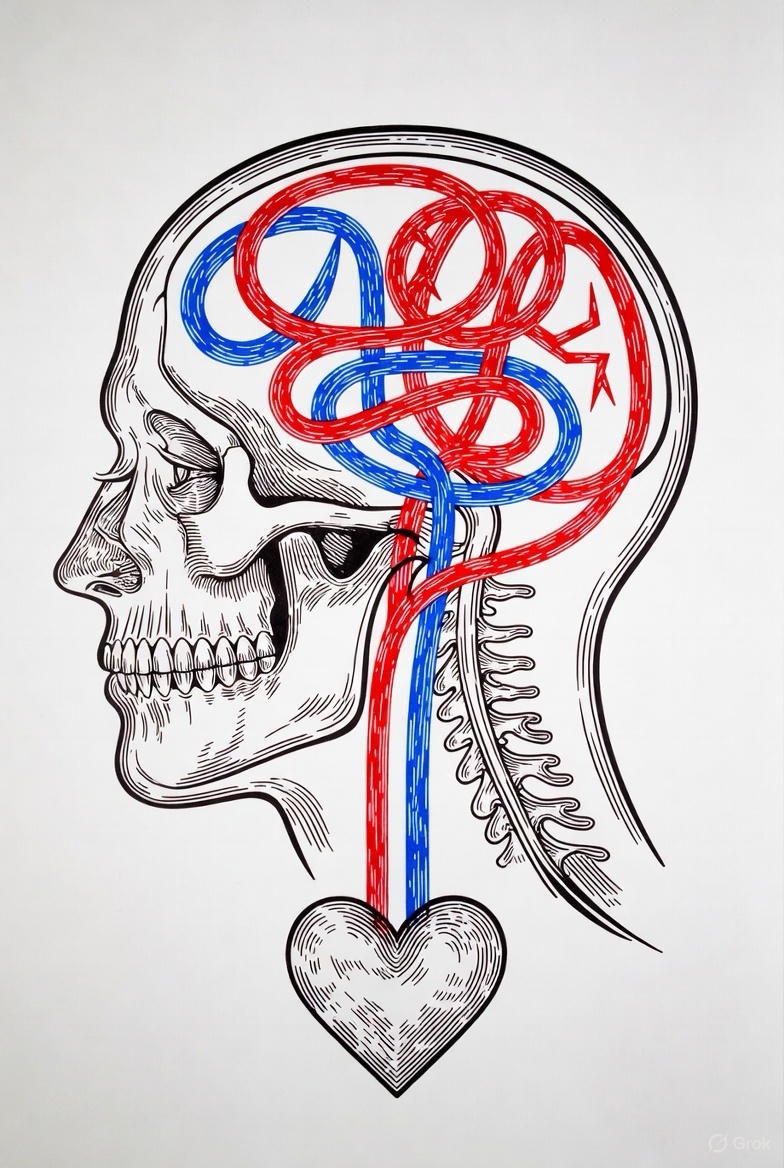
Shared Roots: The Common Ground in the Brain and Body
The link isn’t just behavioral; it’s biological. Depression and anxiety share several underlying mechanisms:
1. Neurotransmitter Imbalance: Both conditions are strongly linked to imbalances in key brain chemicals like serotonin, norepinephrine, and dopamine. These neurotransmitters regulate mood, motivation, fear, and pleasure—meaning a disruption can cause symptoms of both depression and anxiety.
2. The Hyperactive Stress Response: Our body’s central stress response system, the HPA axis (Hypothalamic-Pituitary-Adrenal), is often in overdrive in both disorders. This leads to elevated levels of the stress hormone cortisol, which can contribute to the sleeplessness, agitation, and constant state of “high alert” common in both.
3. Genetics and Temperament: Research suggests that there may be a shared genetic vulnerability that increases the risk for both conditions. Furthermore, an inborn temperament, such as a tendency toward nervousness or behavioral inhibition, can be a risk factor for developing either disorder later in life.
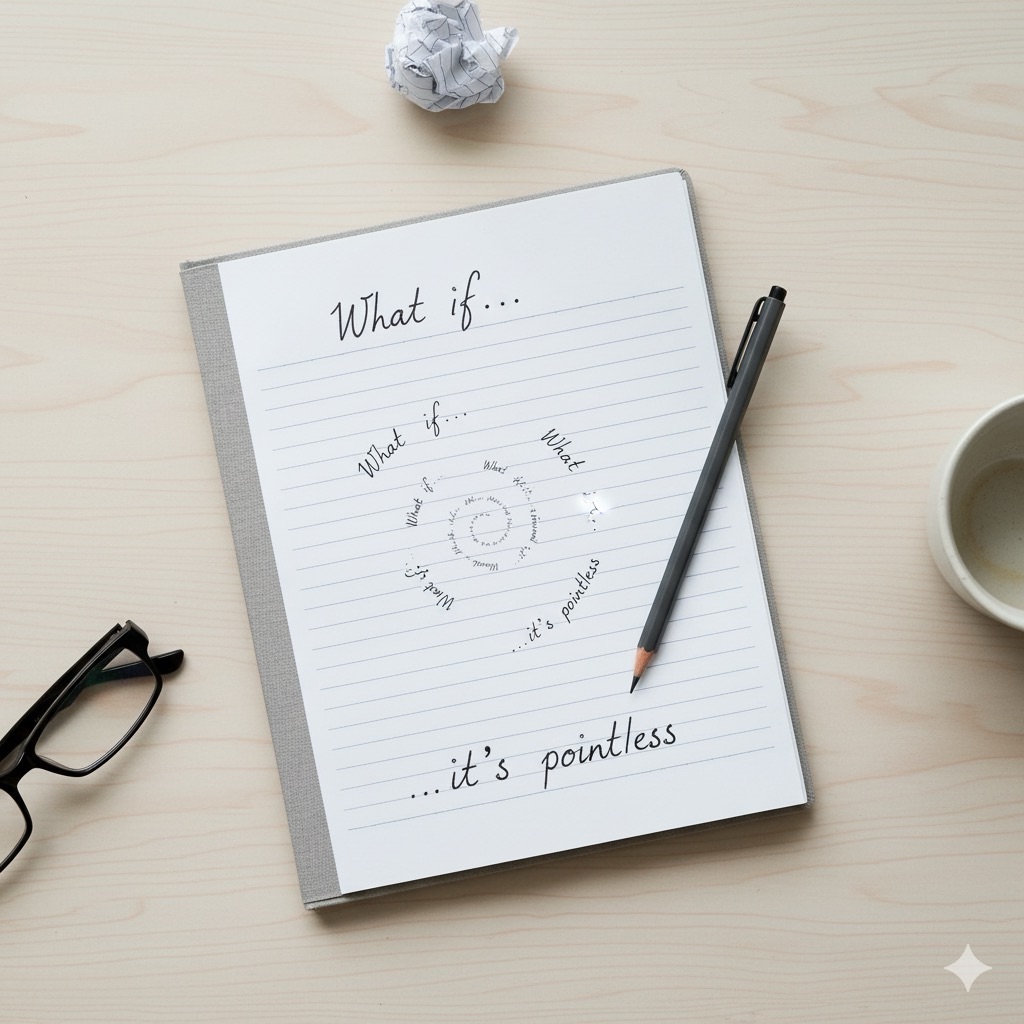
4. Negative Thought Patterns: Both conditions are fueled by a cognitive style known as the “negative triad”: a tendency to have negative views of oneself, the world, and the future. Anxious thoughts (“I’m going to fail this presentation”) can easily spiral into depressive thoughts (“I’m a failure, and my future is doomed”).
Navigating the Overlap: What Does Co-Occurrence Feel Like?
When depression and anxiety co-occur, the experience is unique and often more complex than either alone. You might feel:
· Agitated and Restless, yet Exhausted: Your body is wired, but your mind and spirit are drained.
· Trapped in “What Ifs” and “What’s the Point?”: You’re caught between anxious rumination about the future and a depressive belief that nothing matters.
· Isolated, Yet Fearful of Being Alone: You crave connection but are too anxious to socialize and too depressed to find joy in it.
· Irritable and Impatient: The internal tension from anxiety and the low mood from depression can make you quick to anger or frustration.

Untangling the Knot: Pathways Toward Healing
The good news is that because they are so interconnected, treatment that addresses one often helps the other. The goal isn’t to surgically separate them, but to treat the whole person.
1. Therapy is Key: Certain types of therapy are exceptionally good at tackling both conditions simultaneously.
· Cognitive Behavioral Therapy (CBT): CBT is the gold standard. It helps you identify and reframe the negative thought patterns that fuel both anxiety and depression. You learn to challenge catastrophic thinking (anxiety) and all-or-nothing thoughts (depression).
· Mindfulness-Based Therapies (e.g., MBCT): These therapies teach you to observe your thoughts and feelings without judgment. This can help you break the cycle of getting “hooked” by an anxious thought and spiraling into a depressive state.
2. Medication: Antidepressants, particularly SSRIs (Selective Serotonin Reuptake Inhibitors), are often prescribed because they work on the neurotransmitter systems involved in both depression and anxiety.
3. Lifestyle Foundations: You cannot therapy or medicate your way out of poor self-care. Establishing a routine is a powerful act of rebellion against both disorders.
· Regular Sleep: Prioritize it. Sleep disruption is a major trigger for both.
· Gentle Movement: Exercise is a potent natural antidepressant and anxiety-reducer. A simple daily walk can work wonders.
· Nutrition: Feed your brain and body well. Blood sugar spikes and crashes can mimic or worsen anxiety symptoms.
· Mindfulness and Relaxation: Practices like deep breathing, meditation, or yoga can directly calm the nervous system.

A Final Word of Hope
If you see yourself in this description, please know this: you are not “broken” or “complicated.” You are experiencing a common, though deeply challenging, human condition. The fact that your symptoms are tangled is a clue, not a life sentence.
Reaching out to a therapist or doctor is the first step in unraveling the knot. With the right support and strategies, you can learn to quiet the anxious alarm and lift the depressive fog, reclaiming a life of peace and purpose.
FAQs
Q1: I feel both depressed and anxious at the same time. Is that even possible? Does this mean I have both disorders?

Answer: Absolutely, it is not only possible but very common. This experience is known as comorbidity. It doesn’t necessarily mean you have two entirely separate, distinct disorders. Instead, it often means you are experiencing a “mixed features” presentation where symptoms of both depression and anxiety overlap and interact intensely. Only a qualified professional can give you an official diagnosis, but describing your experience of both sets of symptoms is crucial for getting the right help.
Q2: How can I tell if what I’m feeling is “normal” stress or a clinical issue?
Answer: The key differentiators are intensity, duration, and impairment.
· “Normal” stress or sadness is typically tied to a specific situation, is proportional to the event, and fades as the situation resolves. It might bother you, but it doesn’t completely stop you from functioning.
· Clinical anxiety/depression is often more intense, persistent (lasting for two weeks or more), and can occur without an obvious trigger. The most important sign is that it significantly impairs your life—it affects your work performance, your relationships, your ability to take care of yourself, or your desire to engage in activities you once enjoyed.

Q3: If they are so linked, why do I get a diagnosis of “Major Depressive Disorder” and “Generalized Anxiety Disorder”? Why not one combined diagnosis?
Answer: This is a great question that gets to the heart of how mental health is classified. Our current diagnostic manual (the DSM-5) lists them as separate disorders because they have unique core features. The primary core of Major Depression is a persistent low mood and loss of interest/pleasure. The primary core of Generalized Anxiety is excessive, uncontrollable worry.
However, the system is evolving. The DSM-5 now includes a “specifier” for Major Depression called “with anxious distress,” acknowledging this common overlap. While the labels are separate for clinical precision, any good therapist or doctor will treat you as a whole person, focusing on your unique blend of symptoms.
Q4: Which one should be treated first? The depression or the anxiety?
Answer: In most cases, they are treated simultaneously because the treatments often overlap significantly. For example:
· Cognitive Behavioral Therapy (CBT) effectively targets the negative thought patterns that fuel both conditions.
· SSRI medications (a common class of antidepressants) are also first-line treatments for anxiety disorders.
The goal is not to treat one and then the other, but to use integrated approaches that address the entire cycle. Your treatment plan should be tailored to your most pressing symptoms.
Q5: I’ve heard that anti-anxiety medications (like benzodiazepines) can be addictive. What are the alternatives?
Answer: Your concern is valid. Benzodiazepines (like Xanax or Ativan) can be effective for short-term, acute anxiety but carry a high risk of dependence and tolerance when used long-term.
The preferred, first-line medical treatments are typically:
· SSRIs/SNRIs (Antidepressants): These are not addictive and work on the underlying neurochemical imbalances over time. They help with both depression and anxiety.
· Buspar (Buspirone): This is a non-addictive medication specifically for anxiety.
· Therapy: CBT is considered as effective, if not more effective in the long run, than medication for many anxiety disorders, as it teaches you skills to manage anxiety for life.
Q6: My anxiety feels so physical (heart racing, stomach aches). How is that related to depression?
Answer: This is a critical point often missed. Anxiety is not just “in your head”; it’s a full-body response driven by your nervous system. When you’re anxious, your body releases stress hormones like adrenaline and cortisol, preparing you for “fight or flight.” This causes the physical sensations you describe.
When this system is constantly activated, it’s exhausting. This chronic physical stress can deplete your energy, disrupt your sleep, and wear down your body, directly contributing to the profound fatigue and physical heaviness of depression. So, the physical toll of anxiety is a direct pathway to depressive symptoms.
Q7: What’s the single most helpful thing I can do for myself right now?
Answer: While there’s no magic bullet, one of the most powerful and accessible steps is to practice diaphragmatic (deep belly) breathing.
Why? It directly calms the physiological state of anxiety (slowing your heart rate, lowering blood pressure) and interrupts the panic cycle. By calming your body, you create a small space of relief that can help slow the racing, depressive thoughts. It’s a simple tool you can use anywhere, anytime, to start untangling the knot from the inside.

Q8: I’m in treatment, but I still have bad days. Does this mean it’s not working?
Answer: Not at all. Recovery from depression and anxiety is not a linear process. It’s a journey with ups and downs. Having a bad day or even a bad week is normal and does not mean you’ve failed or that your treatment isn’t working. Progress is measured over weeks and months. The goal is not to eliminate all negative feelings, but to reduce their frequency and intensity and to build the resilience to navigate them more effectively when they do arise.