
When someone you love is living with depression, it can be heartbreaking and confusing. You see them struggling, and your first instinct is to help, to fix it. But often, the words that come with the best intentions can fall flat or even cause harm.
It’s like they’re carrying an invisible weight, and you’re standing beside them, desperately wanting to help carry the load but not knowing how. The good news is that you don’t need to have all the answers. Often, the most powerful thing you can offer is not a solution, but your presence and empathy.
Let’s break down some of the communication do’s and don’ts that can make a world of difference.
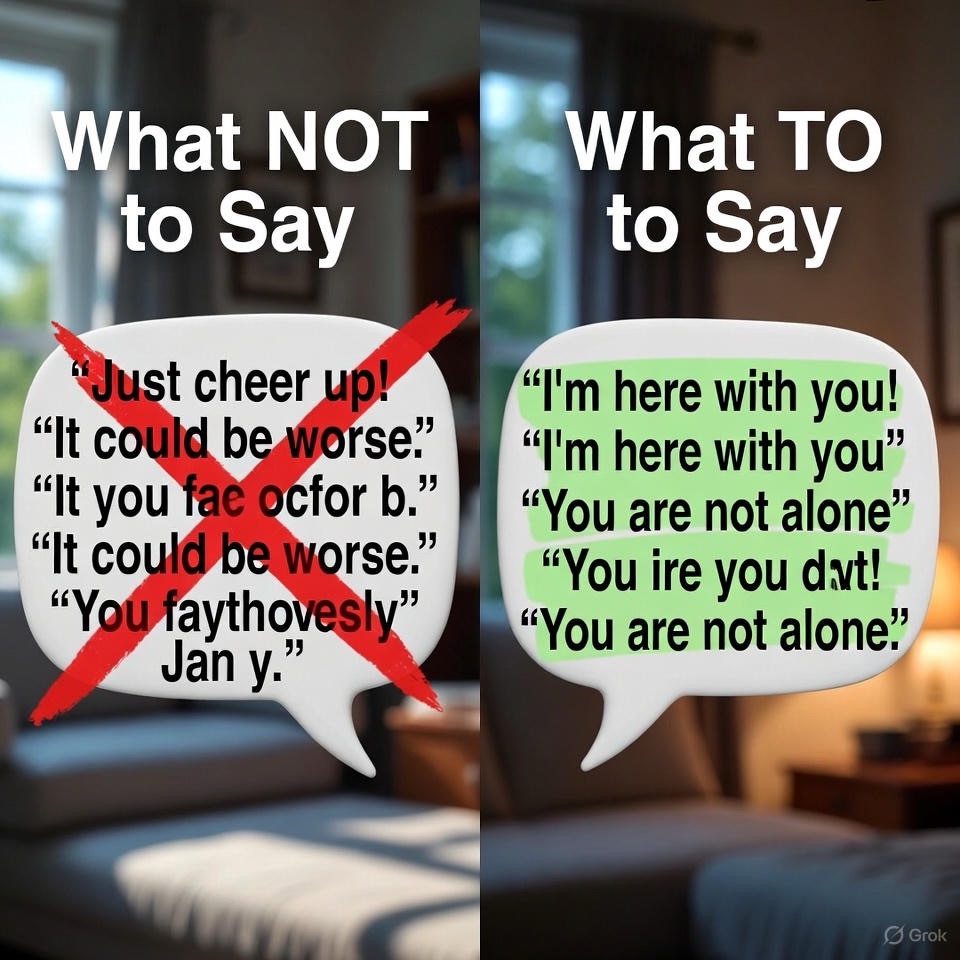
What NOT to Say: The Well-Intentioned Blunders
These phrases are often spoken from a place of love and frustration, but they can invalidate the person’s experience and make them feel more alone.
1. “Just cheer up!” or “Snap out of it!”
· Why it hurts: If they could “snap out of it,” they would. Depression is not a choice or a bad mood; it’s a medical illness. This phrase implies their suffering is voluntary, which can add guilt and shame to their already heavy burden.
2. “You have so much to be happy about.”
· Why it hurts: Depression isn’t logical. A person can have a wonderful job, family, and life on paper and still be clinically depressed. This can make them feel profoundly guilty for their feelings, as if they are failing at being grateful.
3. “It’s all in your head.”
· Why it hurts: While the experience of depression is in the mind, the illness is very real, with physical and neurological components. This phrase dismisses their reality and suggests they are making it up.

4. “What do you have to be depressed about?”
· Why it hurts: This demands a justification for an illness that often doesn’t have a single, clear cause. It forces them to defend their pain and implies their depression isn’t valid.
5. “You just need to exercise/eat better/meditate/go out more.”
· Why it hurts: While lifestyle changes can be part of a management plan, they are not a cure. Offering simplistic solutions minimizes the complex nature of depression and can sound like you’re saying, “Your illness is your fault because you’re not trying hard enough.”
6. Comparing their pain: “I get sad too, but I just push through.”
· Why it hurts: Equating situational sadness with clinical depression is like comparing a puddle to the ocean. It misunderstands the depth, duration, and debilitating nature of the illness.
What TO Say: Phrases That Offer Support and Validation
The goal here is not to fix, but to connect. Your words should communicate, “I see you, I hear you, and I’m here with you.”
1. “You’re not alone. I’m here with you.”
· Why it helps: This is one of the most powerful things you can say. It doesn’t offer a solution, but it offers companionship in their pain, which can alleviate the profound isolation of depression.
2. “I’m sorry you’re going through this. It sounds incredibly hard.”
· Why it helps: This is pure validation. You are acknowledging their struggle without judgment, which makes them feel seen and heard.
3. “Do you want to talk about it? I’m here to listen.”
· Why it helps: It gives them an open invitation to share without pressure. The key is to then actually listen without trying to problem-solve. Sometimes, being a silent, supportive witness is what they need most.

4. “How can I best support you right now?”
· Why it helps: This moves away from assumptions and puts them in control. They might not know the answer, but the question itself shows that you care about their specific needs.
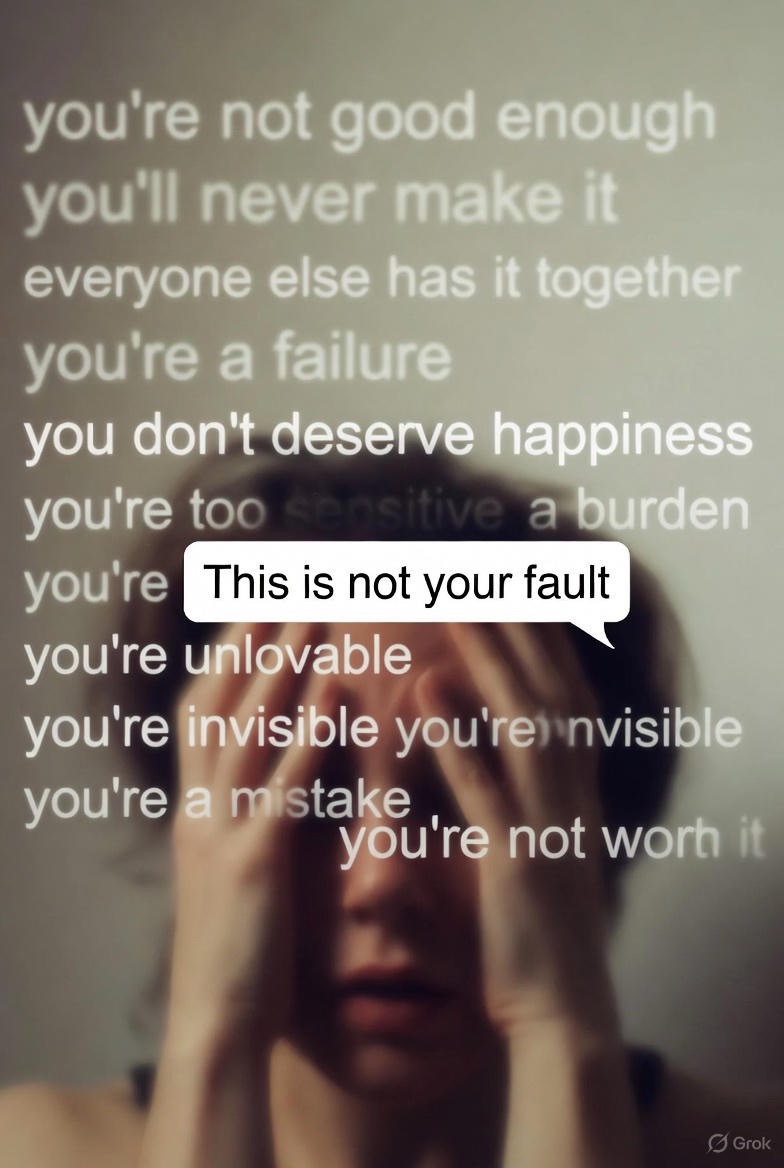
5. “This is not your fault.”
· Why it helps: Depression often comes with a heavy side of self-blame and shame. Directly countering that narrative can be a profound relief.
6. “Would you like some company? We don’t even have to talk.”
· Why it helps: The inertia and fatigue of depression can be overwhelming. Offering low-pressure company—like watching a movie together or just sitting in the same room—can be a comforting reminder that they are cared for.
Beyond Words: The Power of Action
Sometimes, actions speak even louder than these carefully chosen phrases.
· Offer specific help: Instead of “Let me know if you need anything,” try “I’m going to the store, can I pick anything up for you?” or “I made you some soup, I’ll leave it on your porch.” Decision-making is exhausting when you’re depressed.
· Send a check-in text: A simple “Thinking of you. No need to reply!” takes the pressure off them to maintain a conversation.
· Gently encourage professional help: If the time feels right, you could say, “It seems like you’re really carrying a heavy load. Have you thought about talking to someone who is trained to help with this?” Frame it as an act of strength, not weakness.
· Take care of yourself: Supporting someone with depression is draining. You can’t pour from an empty cup. Ensure you have your own support system and practice self-care.

The Bottom Line
You are not their therapist. Your job is not to cure them. Your role is to be a steady, compassionate presence in the storm. By replacing judgment with empathy, and solutions with listening, you become a lifeline—a reminder that even in their darkest moments, they are not alone.

FAQS
Q1: What if I’ve already said the “wrong” thing? I feel terrible.
Answer: Please don’t beat yourself up. Almost everyone who cares about someone with depression has said something well-intentioned that missed the mark. What matters now is what you do next.
· Acknowledge it gently: You can say something like, “I was thinking about what I said the other day, and I realize it might have come across as dismissive. I’m sorry. I’m still learning how to best support you, and I’m here to listen.”
· Focus on the future: Your willingness to learn and do better is what counts. This simple act of acknowledgment can actually strengthen your relationship and build trust, showing that you are a safe person who is genuinely trying.
Q2: They don’t want to talk or see anyone. What do I do then?
Answer: This is one of the most common and frustrating symptoms of depression: social withdrawal. Pushing them to engage often backfires.
· Respect their space, but don’t disappear: Instead of pressuring them, send low-stakes messages. A text saying, “No need to reply, just wanted to say I’m thinking of you,” or “I’m leaving your favorite coffee on the porch. Hope you have an okay day,” can mean the world.
· Offer low-energy companionship: Suggest activities that require little interaction, like watching a movie together in silence, sitting together in the same room while you read, or going for a short, quiet walk. The goal is to make them feel connected without the pressure to “perform” socially.

Q3: How do I know if it’s serious? When should I intervene?
Answer: This is a crucial question. While sadness is a symptom, certain signs indicate a need for more immediate action.
Red flags that require immediate attention include:
· Talking about wanting to die or kill themselves.
· Looking for ways to suicide (e.g., searching for methods online, collecting pills).
· Talking about feeling hopeless, trapped, or being a burden to others.
· Extreme agitation, rage, or recklessness.
· Saying goodbye to people as if for the last time.
What to do in this situation:
· Do not leave them alone.
· Be direct. It’s okay to ask, “Are you thinking about suicide?” This will not put the idea in their head; it will often provide a sense of relief that someone is finally asking.
· Encourage them to contact their therapist or doctor immediately.
· Contact a crisis line: In the US & Canada, you can call or text 988 to reach the Suicide & Crisis Lifeline. In the UK, you can call 111. Other countries have similar services.
· If you believe they are in imminent danger, take them to the nearest emergency room or call for emergency services.
Q4: I feel like I’m walking on eggshells. How can I be honest without triggering them?
Answer: It’s exhausting to constantly monitor your words, and it’s not sustainable for a healthy relationship. The goal isn’t to become a silent ghost, but to shift how you communicate.
· Focus on “I” statements: Instead of saying, “You never want to do anything anymore!” (which sounds accusatory), try, “I miss spending time with you and was wondering if you’d feel up for a short walk with me this weekend?”
· It’s okay to have normal conversations: You can still talk about your day, share a funny story, or discuss a movie. In fact, this can be a welcome distraction. The key is to not get frustrated if they don’t respond with their usual enthusiasm.
· Set gentle boundaries: You can say, “I care about you deeply, and it’s hard for me to hear you say such negative things about yourself. Can we try to talk about what’s underneath those feelings?”

Q5: How do I encourage them to get professional help without sounding like I’m criticizing them?
Answer: This requires sensitivity, as there is still a lot of stigma around therapy and medication.
· Normalize and de-stigmatize: Talk about mental health as a part of overall health. You could say, “Seeing a therapist for depression is like seeing a physical therapist for a back injury. They have the tools to help you heal and get stronger.”
· Frame it as strength: Say, “Asking for help is a sign of incredible strength and self-awareness.”
· Offer practical support: The logistics of finding a therapist can be overwhelming. Offer to help by looking up providers, checking their insurance, or even driving them to the first appointment. This turns your concern into actionable help.
Q6: This is really taking a toll on me. How do I support them without burning out?
Answer: This is not a selfish question; it’s a vital one. You cannot pour from an empty cup. Supporting someone with depression is a marathon, not a sprint.
· Practice self-care without guilt: You need to recharge. Make time for your hobbies, friends, and exercise. You are not abandoning them by taking care of yourself.
· Set your own boundaries: It is okay to say, “I need to take a break for an hour to go for a run, but I’ll call you when I get back.” This models healthy behavior and prevents resentment.
· Find your own support: Talk to a trusted friend or a therapist of your own. Joining a support group for family and friends of people with mental illness can be incredibly validating, as you’ll connect with others who truly understand your experience.

Q7: What if they get angry or push me away when I try to help?
Answer: Try not to take it personally. Irritability and anger are common symptoms of depression. They are often angry at their own situation and internal pain, and it spills out onto the people closest to them.
· Don’t engage in an argument: You can say, “I can see you’re really upset right now. I’m going to give you some space, but I’m still here for you.”
· Re-establish contact later: Once things have calmed down, you can check in. The consistent message should be, “Even when you push me away, I’m not going to abandon you.” This reliability is a powerful anchor for someone who feels they are pushing everyone away.

