A simple cut or scrape is usually a minor inconvenience. But what happens when that small wound becomes infected with something far more dangerous than ordinary bacteria? Welcome to the world of MRSA—a silent, antibiotic-resistant threat that can turn a minor injury into a serious medical emergency.
What is MRSA?
MRSA (pronounced MER-suh) stands for Methicillin-Resistant Staphylococcus aureus. Let’s break that down:
· Staphylococcus aureus: A common type of bacteria (staph) that many people carry on their skin or in their nose without getting sick.
· Methicillin-Resistant: This strain has evolved to survive treatment with common antibiotics like methicillin, penicillin, and amoxicillin.
Think of MRSA as a “superbug”—a regular staph infection that has learned to wear armor against our usual medical weapons.
How MRSA Infects Wounds: The Open Door Policy
MRSA doesn’t create wounds; it exploits them. Any break in your skin serves as an open invitation:
· Cuts and scrapes
· Surgical incisions
· Burns
· Insect bites
· Even tiny cracks in dry skin or irritation from shaving
Once inside, MRSA multiplies rapidly. Because it’s resistant to many antibiotics, your body’s defenses and standard treatments may struggle to contain it, leading to serious complications.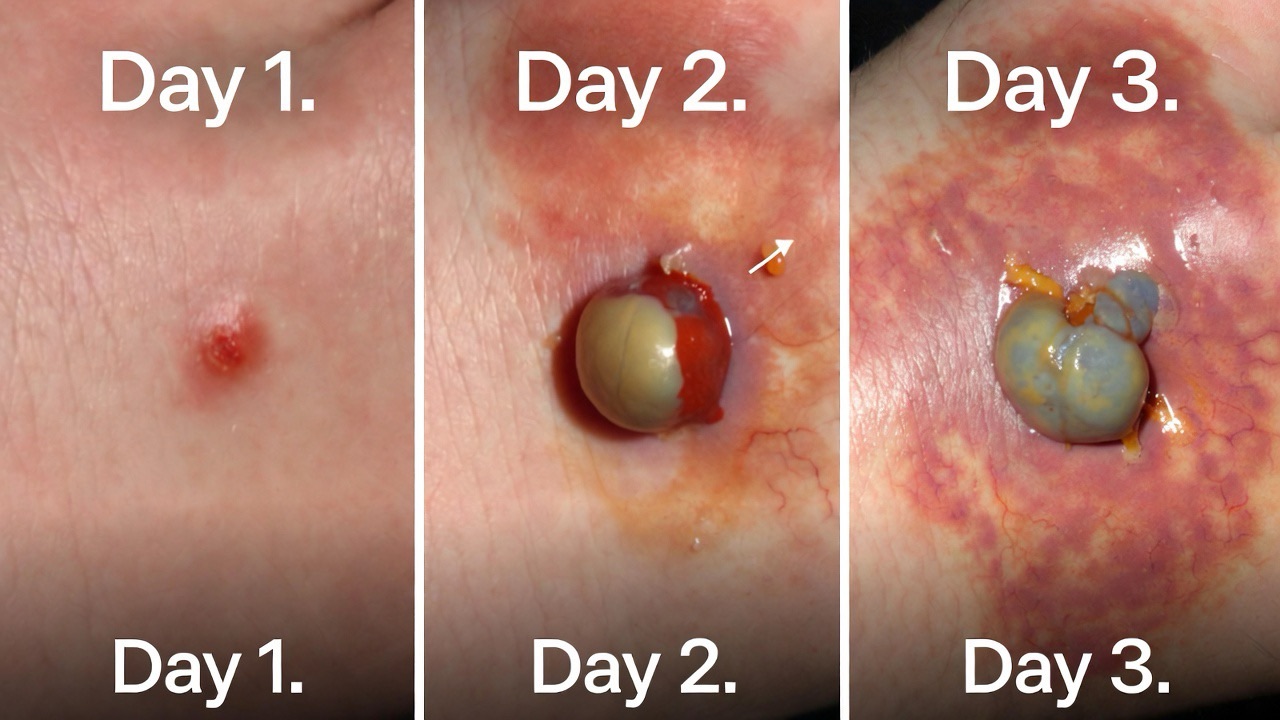
Spotting a MRSA Infection: Not Your Average Infection
While any infected wound can be red, swollen, and painful, MRSA infections often have distinctive characteristics:
Early Signs:
· Red, swollen, painful area on the skin
· May resemble a spider bite, pimple, or boil
· Often warm to the touch
· May have pus or other drainage
Warning Signs of Serious Infection:
· The affected area grows rapidly (sometimes within hours)
· Fever and chills
· The center of the infection softens and fills with pus (becomes an abscess)
· Red streaks extending from the wound
· The infection doesn’t improve after using over-the-counter antibiotic ointments
Critical Distinction: While a normal infected wound might improve with basic care, a MRSA infection typically worsens quickly and doesn’t respond to standard antibiotic creams.
Who is Most at Risk?
While anyone can get MRSA, some factors increase vulnerability:
Community-Associated MRSA (CA-MRSA):
· Athletes (especially in contact sports)
· Children in daycare
· Military personnel in barracks
· People living in crowded conditions
· Anyone sharing personal items (razors, towels, athletic equipment)
Healthcare-Associated MRSA (HA-MRSA):
· Recent hospitalization or surgery
· Residents of long-term care facilities
· People with medical tubes or catheters
· Those with weakened immune systems
The Treatment Challenge: When Standard Antibiotics Fail
Treating MRSA requires a different approach than typical wound infections:
For Skin and Soft Tissue Infections:
1. Incision and Drainage: The primary treatment for MRSA abscesses. A healthcare provider makes a small cut to drain the pus completely. This is often more crucial than antibiotics.
2. Specific Antibiotics: Doctors prescribe antibiotics that still work against MRSA, such as trimethoprim-sulfamethoxazole, doxycycline, or clindamycin.
3. Wound Care: Meticulous cleaning, dressing changes, and monitoring for spread.
For Serious/Systemic Infections:
· Intravenous (IV) antibiotics in a hospital setting
· Possible combination of antibiotics
· Surgical intervention for deep infections
· Long-term treatment plans for recurrent infections
Important: Never attempt to drain a suspected MRSA infection yourself. This can push bacteria deeper into tissue or spread it to others.
Prevention: Your Best Defense Against MRSA
Since MRSA is difficult to treat, prevention is absolutely critical:
For Everyone:
1. Hand Hygiene: Wash hands frequently with soap and water for at least 20 seconds. Alcohol-based sanitizers are effective when washing isn’t possible.
2. Wound Protection: Keep cuts and scrapes clean and covered with sterile, dry bandages until healed.
3. No Sharing: Avoid sharing personal items like towels, razors, clothing, or athletic equipment.
4. Clean Surfaces: Regularly disinfect high-touch surfaces, especially in gyms or shared spaces.
5. Shower After Contact: Shower immediately after activities involving skin-to-skin contact.
For Healthcare Settings:
· Healthcare workers should follow strict hand hygiene protocols
· Proper use of gloves and gowns when treating infected wounds
· Isolation precautions for infected patients
· Thorough cleaning of patient rooms and equipment
When to Seek Medical Attention: The Emergency Red Flags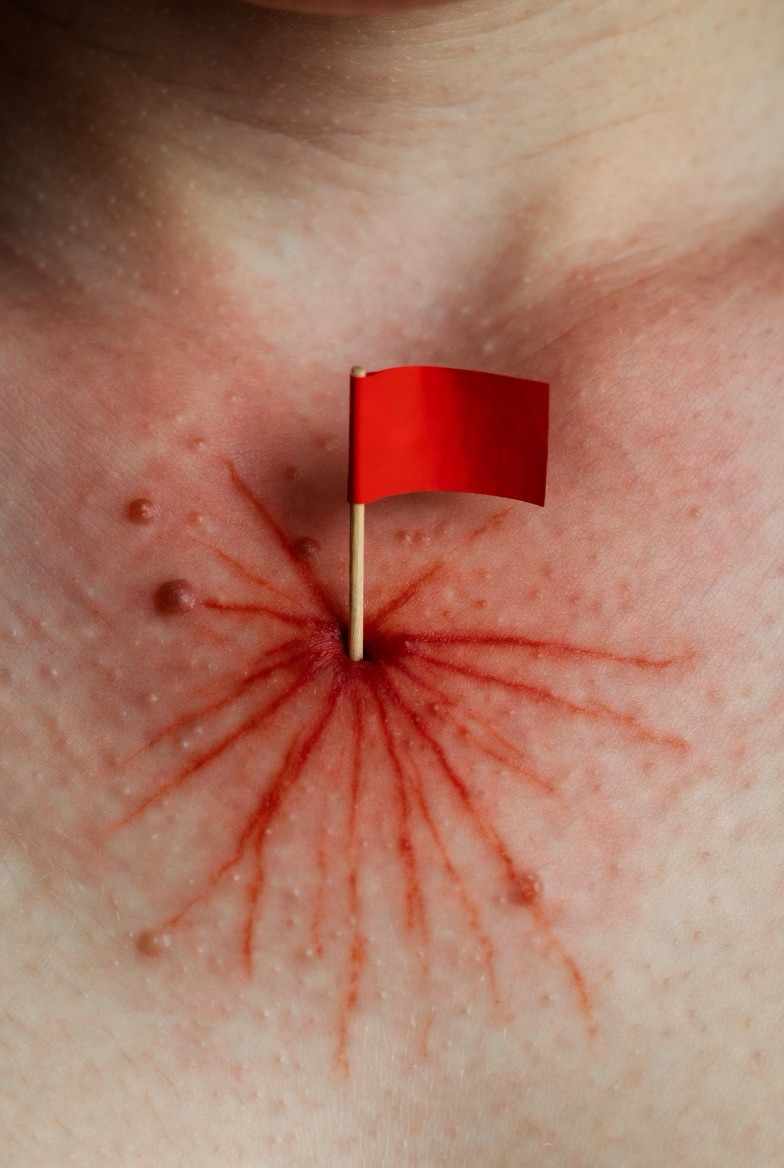
Don’t wait if you notice any of these warning signs:
· A wound infection that’s spreading rapidly
· Fever accompanying a skin infection
· The infected area is large, very painful, or has red streaks
· The infection is near your eyes, mouth, or on your face
· You have a weakened immune system or chronic illness (like diabetes)
· The infection isn’t improving after 48 hours of proper care
Emergency Symptoms (Go to ER Immediately):
· High fever (over 101°F) with chills
· Confusion or dizziness
· Rapid heartbeat or breathing difficulties
· The infected area turns dark purple or black
· Spreading redness that’s moving quickly
Living With Recurrent MRSA Infections
Some people become MRSA “carriers,” meaning the bacteria lives on their skin or in their nose without causing infection. If you experience recurrent MRSA infections, your doctor might recommend:
· Decolonization protocols (special soap and ointment)
· Changing your personal hygiene routine
· Environmental cleaning measures for your home
· Testing family members who might be carriers
The Bigger Picture: Antibiotic Resistance and Responsible Use
MRSA didn’t develop in a vacuum. The overuse and misuse of antibiotics has accelerated the development of resistant bacteria like MRSA. You can help combat this global health threat by:
· Never demanding antibiotics for viral infections (like colds or flu)
· Taking prescribed antibiotics exactly as directed (complete the full course)
· Never sharing or using leftover antibiotics
· Talking to your doctor about antibiotic stewardship
The Bottom Line: Respect, Don’t Panic
MRSA is a serious infection that demands respect, but not panic. Most healthy people who develop a MRSA skin infection recover completely with proper medical treatment. The key is awareness and prompt action.
Remember this formula:
Unhealing Wound + Rapid Worsening + Possible Fever = Time to See a Doctor Immediately
Protect your wounds, practice good hygiene, and don’t ignore infections that behave unusually. In the battle against superbugs like MRSA, an informed and proactive approach is your most powerful weapon.
FAQs
Q1: How do I know if my wound is infected with MRSA or just a normal infection?
A: While only a lab test can confirm MRSA, there are warning signs that suggest it might be more than a typical infection:
· Rapid Worsening: The area gets bigger, more painful, and more swollen within hours or a day or two.
· “Spider Bite” Look: Often starts looking like a bug bite or a pimple that quickly turns into a painful, deep lump.
· Abscess Formation: Frequently forms a pus-filled head or a soft center.
· Fever: Developing a fever alongside a skin infection is a significant red flag.
· No Response to OTC Creams: Doesn’t improve with over-the-counter antibiotic ointments.
Bottom line: If your wound infection is behaving aggressively or unusually, see a doctor promptly.
Q2: Can I get MRSA from a tattoo or piercing?
A: Yes, absolutely. Any procedure that breaks the skin carries a risk if proper sterilization isn’t followed. MRSA can be introduced via contaminated needles, ink, or equipment. To minimize risk:
· Choose a licensed, professional, and reputable studio.
· Ensure they use single-use, sterile needles and ink caps.
· They should wear gloves and follow strict hygiene protocols.
· Follow all aftercare instructions meticulously to prevent infection.
Q3: Is MRSA contagious? How does it spread?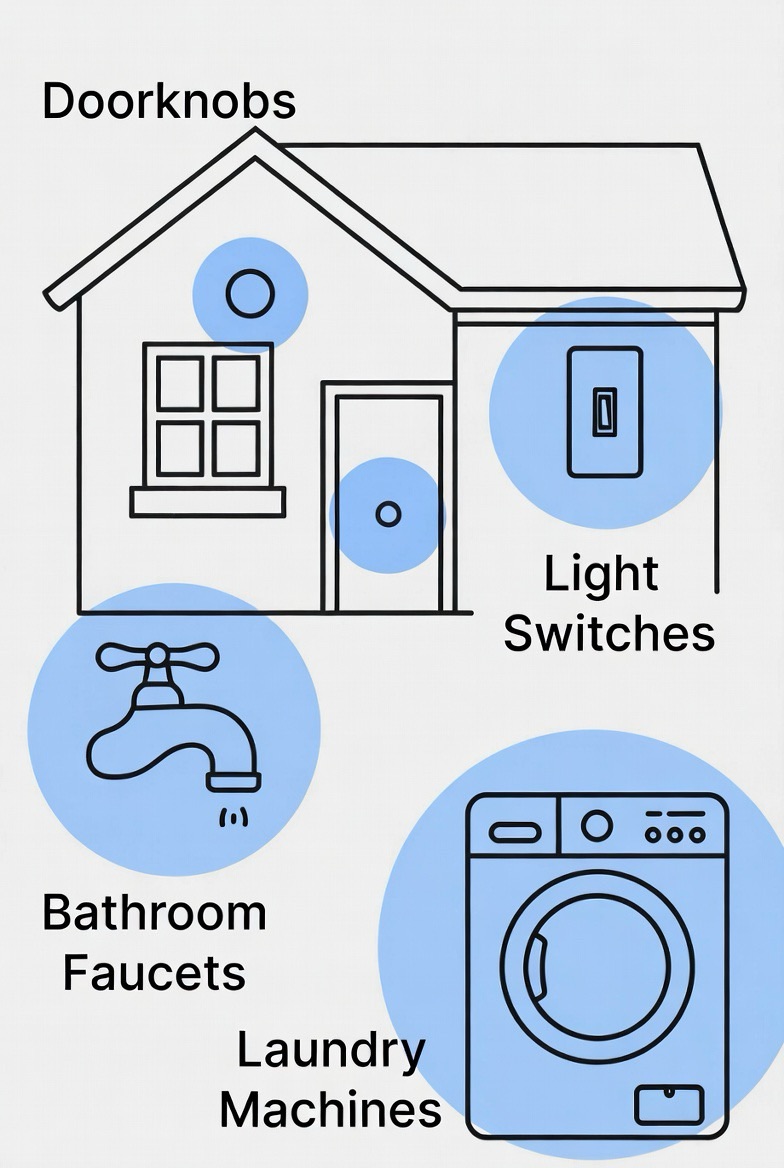
A: Yes, MRSA is contagious. It spreads primarily through:
· Direct Contact: Skin-to-skin contact with someone who has an active infection or is a carrier.
· Contaminated Objects: Touching surfaces or items contaminated with the bacteria (e.g., shared towels, razors, athletic equipment, gym benches, or bed linens).
· Poor Hygiene: Not washing hands properly after touching an infected wound or a contaminated surface.
Q4: If someone in my household has MRSA, how do I protect myself and clean the house?
A: Focus on hygiene and targeted cleaning:
· Hand Hygiene: Wash hands frequently with soap and water. Use alcohol-based hand sanitizer.
· No Sharing: Do not share personal items like towels, washcloths, razors, clothing, or bedding.
· Laundry: Wash the infected person’s clothes, towels, and linens separately in hot water and dry them on high heat.
· Disinfect Surfaces: Regularly clean high-touch surfaces (doorknobs, light switches, countertops, bathroom fixtures) with an EPA-registered disinfectant that states it kills MRSA.
· Cover Wounds: Ensure any draining wounds are kept covered with clean, dry bandages.
Q5: Once I’ve had a MRSA infection, am I immune to it?
A: No. Having a MRSA infection does not make you immune. In fact, you can get re-infected. Some people also become “carriers” or are “colonized,” meaning the bacteria lives on their skin or in their nose without making them sick, but they can still spread it to others or to a new wound on their own body.
Q6: My doctor drained my abscess but didn’t prescribe antibiotics. Is that normal?
A: Yes, this is often standard and correct treatment. For uncomplicated skin abscesses, incision and drainage (I&D) is the primary and most effective treatment. If the infection hasn’t spread and you are otherwise healthy, completely draining the pus may be all that’s needed. Antibiotics are added if the infection is severe, has spread, or you have a weakened immune system.
Q7: What is the “decolonization” process I’ve heard about for recurrent MRSA?
A: Decolonization is a protocol to reduce the amount of MRSA bacteria on a person’s skin and in their nose to prevent recurring infections. It is typically used for people with repeated MRSA issues and may involve a 5-10 day regimen of:
· Special Wash: Using an antiseptic body wash (like chlorhexidine) daily.
· Nasal Ointment: Applying a prescription antibiotic ointment (like mupirocin) inside the nostrils.
· Environmental Measures: Decontaminating personal items and bedding as outlined above.
Important: This should only be done under a doctor’s direction.
Q8: Are there any new antibiotics that work against MRSA?
A: Yes, there are antibiotics that are effective against MRSA, though resistance is an ongoing battle. Common oral options include trimethoprim-sulfamethoxazole, doxycycline, and clindamycin. For severe infections, intravenous (IV) antibiotics like vancomycin, daptomycin, or linezolid are used. Researchers are constantly developing new drugs, but using all antibiotics responsibly is key to preserving their effectiveness.
Q9: Can I go to work or school with a MRSA infection?
A: It depends on the situation. Generally:
· You CAN go if the infection can be kept completely covered with a clean, dry bandage and you practice strict hygiene.
· You should likely STAY HOME if the wound is draining and cannot be contained, if you work in healthcare/food service/childcare with direct contact, or if you have a fever.
· Always inform your workplace or school nurse, especially if you are in a high-risk setting. They will have specific policies.
Q10: Is there a vaccine for MRSA?
A: No, there is currently no commercially available vaccine to prevent MRSA infections. Development has been challenging due to the complex nature of the bacteria. Prevention relies entirely on the hygiene and proactive measures outlined in the article.
Q11: My child got MRSA from wrestling. Will they always be at risk?
A: They will be at higher risk as long as they participate in contact sports, but the risk can be managed aggressively:
· Skin Checks: Coaches and athletes should do daily skin checks.
· Cover All Wounds: Any scrape or sore must be covered with a bio-occlusive bandage (seals on all sides) before practice or meets.
· No Sharing: Absolutely no sharing of towels, gear, uniforms, or water bottles.
· Hygiene: Shower immediately after practice with soap and water.
· Clean Equipment: Disinfect mats and gear after every use.
Q12: What’s the difference between “colonized” and “infected” with MRSA?
A: This is a crucial distinction:
· Colonized (Carrier): The MRSA bacteria is present on the skin or in the nose but is not causing illness or symptoms. The person is generally healthy but can spread the bacteria.
· Infected: The MRSA bacteria has entered the body (usually through a wound) and is actively causing an illness, such as a skin infection, pneumonia, or bloodstream infection. This requires treatment.

