Imagine waking up with a painful, swollen lump on your skin that’s warm to the touch and getting bigger by the day. Chances are, you might be dealing with an abscess. While they’re common, abscesses can range from a minor nuisance to a serious medical concern. Let’s break down what they are, why they happen, how to treat them, and when it’s time to head to the emergency room.

What Is an Abscess?
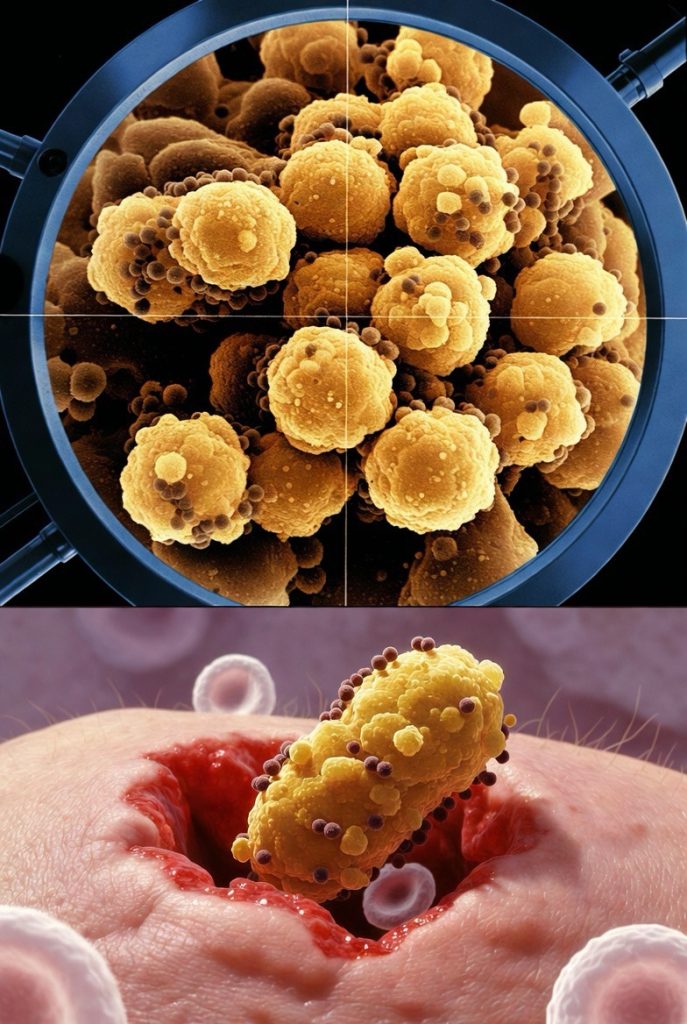
An abscess is a localized collection of pus that forms within body tissue. It’s essentially your immune system’s way of walling off an infection to prevent it from spreading. The pus inside is a thick fluid made up of dead white blood cells, bacteria, and tissue debris.
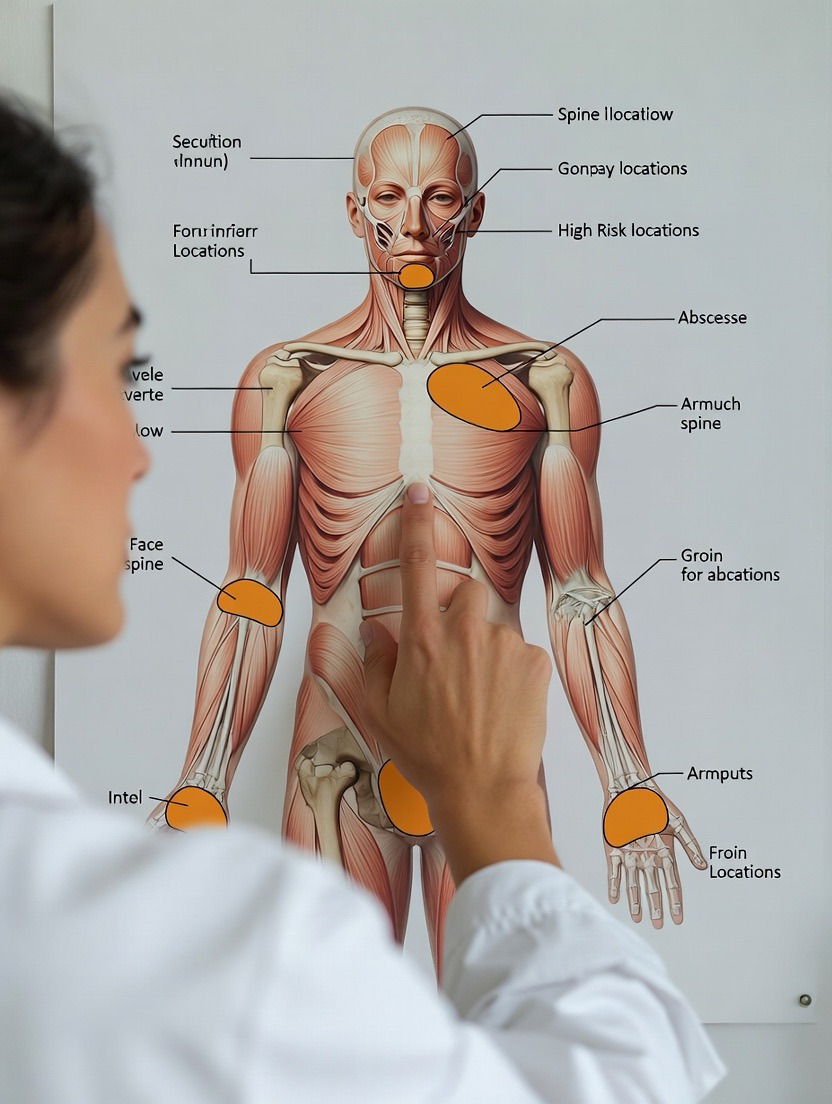
Abscesses can occur anywhere on the body, both externally and internally. Common types include:
· Skin abscesses: Such as boils or carbuncles.
· Dental abscesses: In the teeth or gums.
· Internal abscesses: In organs like the liver, brain, or appendix (less common but more serious).
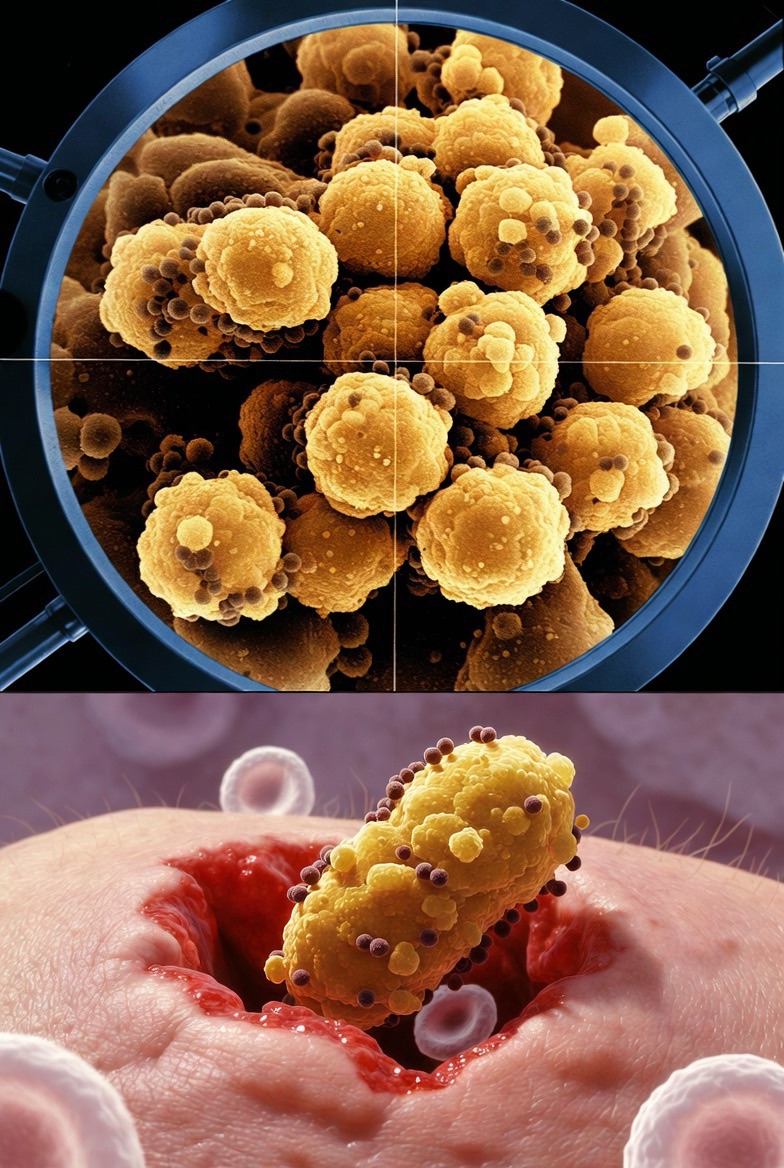
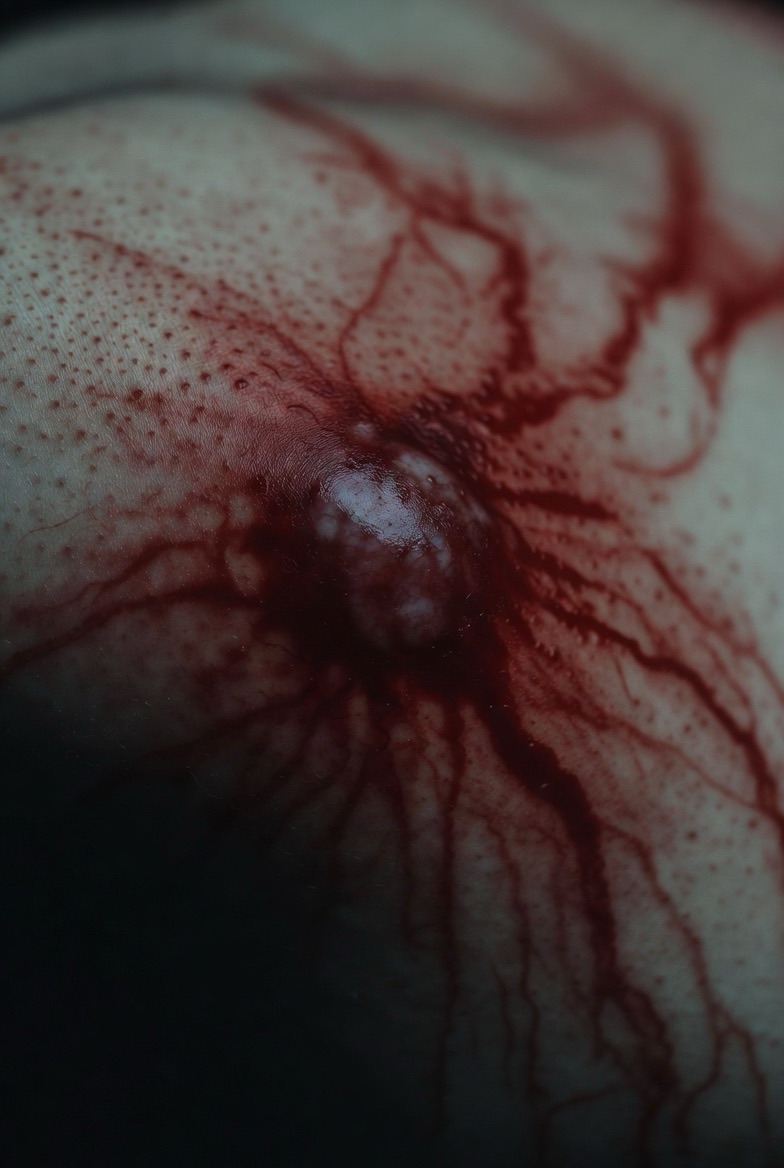
They often appear as swollen, red, painful bumps and may feel warm. Some even develop a visible “head” of pus.
What Causes an Abscess?
Abscesses are typically caused by a bacterial infection, most commonly by Staphylococcus aureus, including the antibiotic-resistant strain MRSA. Here’s how they develop:
1. Bacterial Invasion: Bacteria enter through a break in the skin—a cut, scrape, ingrown hair, or blocked sweat gland.
2. Immune Response: Your body sends white blood cells to fight the infection.
3. Pocket Formation: Tissue dies, creating a cavity that fills with pus, forming the abscess.
Risk Factors:
· Poor hygiene
· Compromised immune system (e.g., from diabetes, chemotherapy, or HIV)
· Skin conditions like eczema
· Close contact with someone who has a staph infection
· Intravenous drug use
How Are Abscesses Treated?
Important: Never try to squeeze or “pop” an abscess at home. This can push bacteria deeper, spread the infection, or lead to serious complications.

Professional Medical Treatment:
· Incision and Drainage (I&D): This is the primary treatment. A healthcare provider numbs the area, makes a small cut, and drains the pus. Sometimes, packing gauze is placed to help it heal from the inside out.
· Antibiotics: Prescribed if the infection is severe, has spread, or if you have a weakened immune system. They are often used in conjunction with drainage.
· Pain Management: Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage discomfort.
At-Home Care After Treatment:

· Keep the area clean and dry.
· Change dressings as directed.
· Take all prescribed antibiotics, even if you start feeling better.
· Apply warm compresses to encourage drainage and soothe the area.
When to Seek Emergency Care

While many abscesses can be treated in a doctor’s office, some situations require immediate medical attention. Go to the ER if you experience:
1. Fever and Chills: This can indicate the infection is spreading into your bloodstream (sepsis).
2. Rapid Growth or Extreme Pain: The abscess is enlarging quickly or is unbearably painful.
3. Location Concerns: An abscess on the face, spine, groin, or rectal area can be more dangerous.
4. Systemic Symptoms: Nausea, vomiting, rapid heart rate, or confusion.
5. Underlying Conditions: If you have diabetes, a weakened immune system, or peripheral vascular disease.
6. No Improvement: After drainage, if redness, swelling, or pain increases.
7. Signs of Spreading Infection: Red streaks extending from the abscess (lymphangitis).
Prevention Tips
Preventing abscesses often comes down to good hygiene and skin care:
· Wash hands regularly with soap and water.
· Clean cuts and scrapes immediately and keep them covered.
· Avoid sharing personal items like razors or towels.
· Manage chronic health conditions effectively.
· Seek prompt care for skin infections before they worsen.
The Bottom Line
An abscess is more than just a painful bump—it’s a sign your body is fighting an infection. While common and often manageable with proper medical care, ignoring it or attempting home surgery can lead to serious complications. Listen to your body: if you’re unsure, or if symptoms escalate, don’t hesitate to contact a healthcare provider. Your health and safety always come first.
If you suspect you have an abscess, reach out to your doctor or urgent care clinic for an evaluation. When in doubt, especially with severe symptoms, head to the nearest emergency room.

FAQs
Q1: Can an abscess go away on its own without treatment?
A: Occasionally, a very small abscess might drain spontaneously and heal. However, most abscesses require medical intervention because the wall of pus prevents antibiotics from reaching the infection effectively. Without proper drainage, an abscess can linger, grow, and risk spreading the infection. It’s always safest to have a healthcare professional evaluate it.
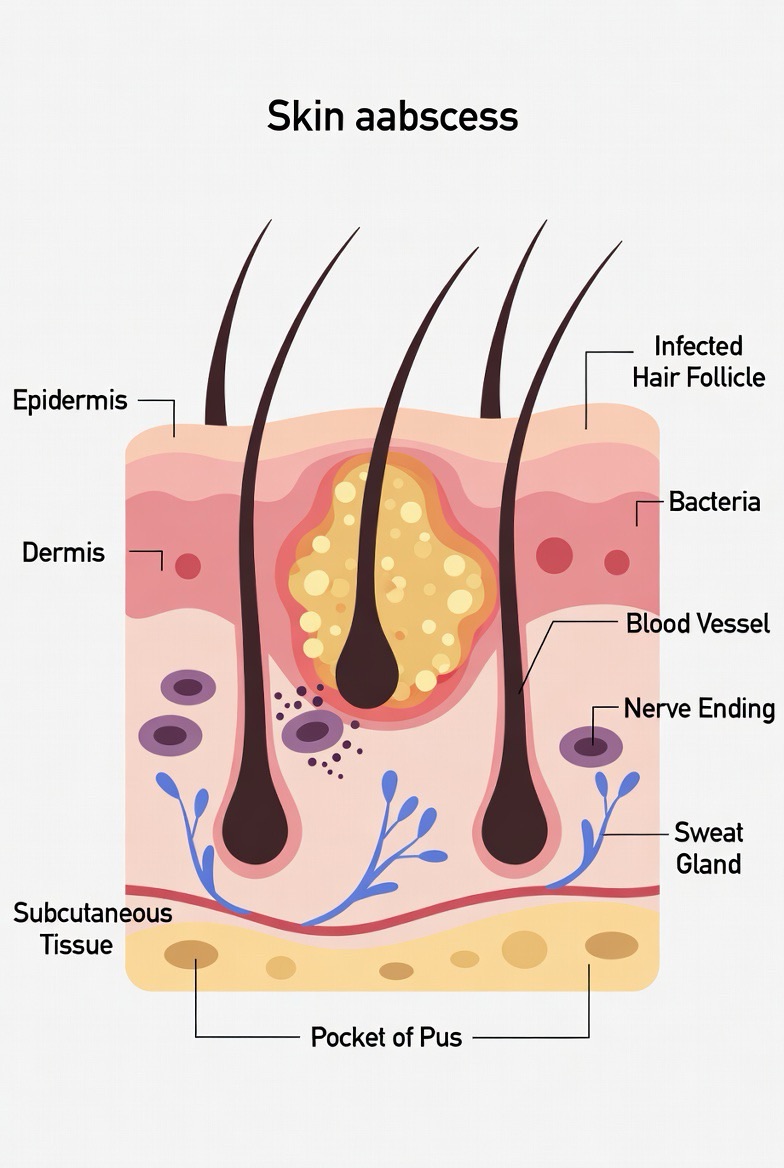
Q2: What’s the difference between an abscess and a boil?
A: A boil (or furuncle) is a type of skin abscess. It specifically starts in a hair follicle or oil gland. A carbuncle is a cluster of boils. “Abscess” is the broader term for any walled-off collection of pus in the body, which can include boils but also internal abscesses (e.g., in the liver) or dental abscesses.
Q3: Is it safe to pop an abscess at home with a sterile needle?
A: No, it is not safe. Even with a sterilized needle, you risk:
· Pushing the infection deeper into your tissue.
· Causing a much wider, more dangerous infection (cellulitis).
· Introducing new bacteria.
· Incomplete drainage, leading to a recurrence.
· Severe bleeding if you hit a blood vessel.
Incision and drainage is a medical procedure that should be performed by a trained professional, often with anesthesia and proper aftercare.
Q4: Why do I need antibiotics if the abscess is drained?
A: Drainage removes the pus, which is the core of the infection. However, antibiotics may still be prescribed if:
· The infection has spread to the surrounding skin.
· You have multiple abscesses.
· You have a high fever or signs of systemic infection.
· The abscess is in a high-risk area (like the face).
· You have a condition that weakens your immune system (e.g., diabetes).
Q5: What should I do if the abscess is draining on its own?
A:
1. Keep it clean: Gently wash the area with mild soap and warm water.
2. Cover it: Use a clean bandage or gauze to absorb the drainage and prevent bacteria from spreading.
3. Do NOT squeeze: Let it drain naturally.
4. Apply warm compresses: This can help encourage complete drainage.
5. Seek medical care: Even if it’s draining, a doctor should assess it to ensure all infected material is removed and to provide appropriate wound care instructions.

Q6: How can I tell if an abscess is infected versus just inflamed?
A: An abscess is an infection by definition. The signs of infection are precisely what characterize it: pain, redness, warmth, and swelling. The key escalation to watch for is when the local infection shows signs of spreading systemically (throughout the body), such as fever, chills, nausea, or red streaks leading from the site.
Q7: Are abscesses contagious?
A: The pus inside an abscess contains bacteria. Direct contact with the drainage can potentially spread the bacteria to another person, especially if they have a break in their own skin. It’s crucial to keep a draining abscess covered with a clean bandage, practice excellent hand hygiene, and avoid sharing personal items like towels or razors.
Q8: How long does it take for an abscess to heal after drainage?
A: Healing time varies by size and location. After professional drainage:
· Immediate pain relief is common once pressure is released.
· The wound may be packed with gauze, which needs changing regularly for a few days.
· Most small to medium skin abscesses heal within 1-2 weeks.
· It’s crucial to follow all aftercare instructions and complete any course of antibiotics.
Q9: Why do I keep getting recurrent abscesses (e.g., in the groin or underarms)?
A: Recurrent abscesses in areas like the groin (hidradenitis suppurativa) or underarms may point to an underlying condition, not just a simple infection. Potential causes include:
· Chronic skin conditions (like hidradenitis suppurativa).
· Being a carrier of Staph bacteria.
· Medical conditions such as uncontrolled diabetes or obesity.
· Close shaving, which can irritate hair follicles.
A primary care doctor or dermatologist can help diagnose the root cause and develop a long-term management plan.
Q10: Can I prevent abscesses from forming?
A: While not all are preventable, you can significantly reduce your risk:
· Practice good hygiene: Wash hands and skin regularly.
· Treat wounds immediately: Clean cuts/scrapes and apply antibiotic ointment and a bandage.
· Avoid sharing personal items: Razors, towels, and athletic equipment.
· Manage health conditions: Keep diabetes well-controlled and maintain a healthy weight.
· Don’t pick or squeeze: Pimples or minor skin irritations.