Antibiotics are one of modern medicine’s greatest miracles. But like any powerful tool, they must be used correctly. Misusing them doesn’t just harm you—it threatens public health for everyone by fueling antibiotic resistance. Here’s a simple, vital guide to using antibiotics the right way, explained in plain terms.
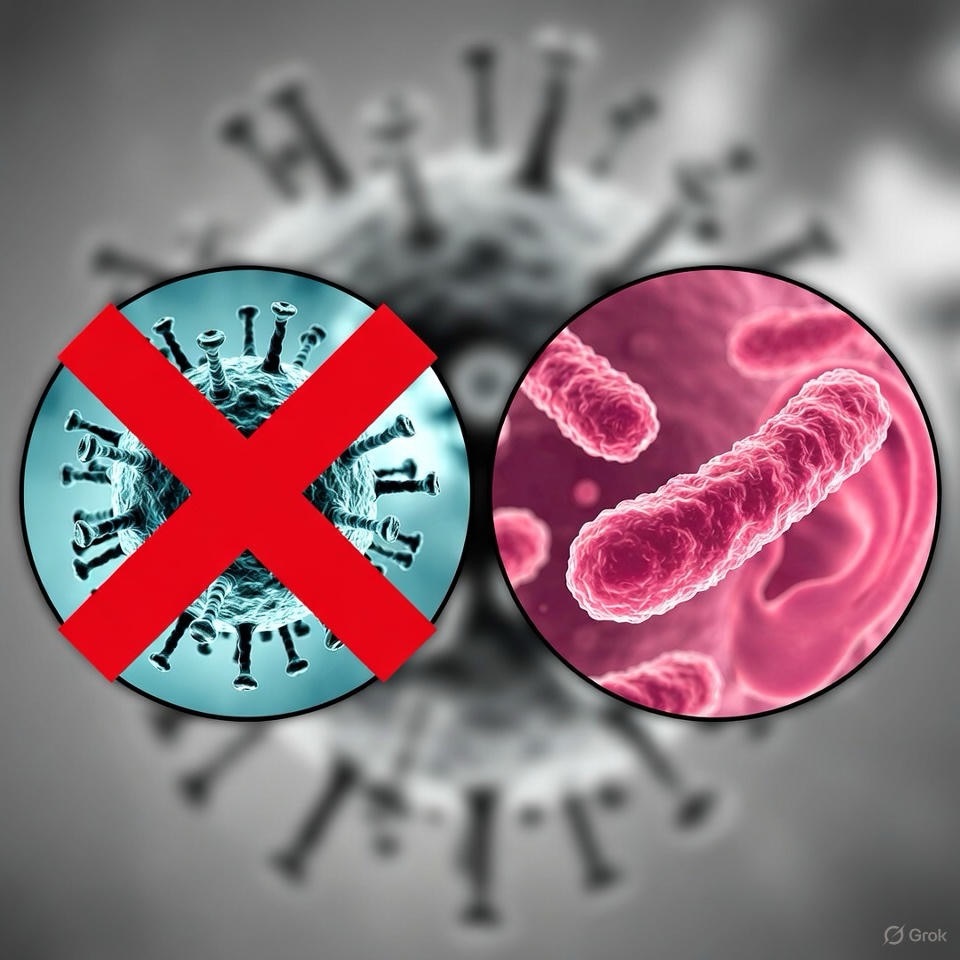
The Core Problem: What is Antibiotic Resistance?
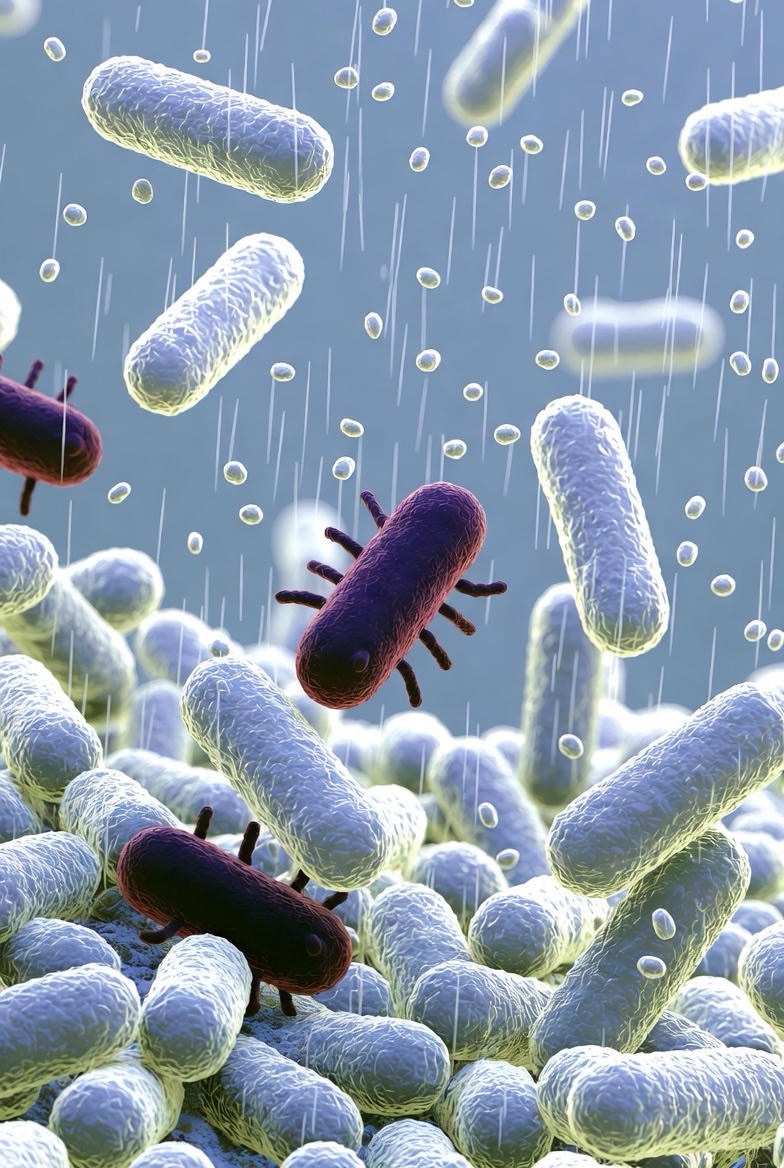
Imagine antibiotics as a specialized army sent to kill bacterial invaders. When you use them incorrectly—by taking too little, stopping early, or using them for the wrong enemy (like a virus)—you allow the strongest, smartest bacteria to survive. These survivors then multiply, creating new generations of “superbugs” that the original antibiotic can no longer defeat. This is antibiotic resistance.
The frightening result? Common infections like pneumonia, urinary tract infections, or skin infections could become untreatable again. This isn’t a future scare; it’s a current global health crisis.
The Do’s: Your Responsibility as a Patient

DO take the antibiotic exactly as prescribed. This means the right dose at the right time (e.g., “every 8 hours”) for the full course (e.g., “for 10 days”), even if you feel better in 3 days. The prescription length is calculated to fully eradicate the infection.
DO finish the entire course. This is non-negotiable. Stopping early is the perfect recipe for breeding resistant bacteria. Completing the course ensures no hardy survivors are left to multiply.
DO take them with a full glass of water, unless your doctor or pharmacist gives other instructions. Some require food to avoid stomach upset; others work best on an empty stomach. Always ask.

DO store them properly. Most antibiotics need to be kept in a cool, dry place (not the humid bathroom cabinet). Some liquid forms require refrigeration—check the label.
DO report any severe side effects to your doctor immediately. While some stomach upset is common, severe diarrhea, rash, or signs of an allergic reaction (swelling, difficulty breathing) need urgent attention.
The Don’ts: The Missteps That Fuel Resistance

DON’T pressure your doctor for antibiotics for a cold or flu. These are caused by viruses. Antibiotics only work against bacterial infections. Using them for viruses is useless and dangerous.
DON’T skip doses or double up. Skipping a dose gives bacteria a chance to regroup. Doubling up to “catch up” increases your risk of side effects without improving efficacy. Set an alarm if you have trouble remembering.
DON’T save leftover pills for “next time.” Each infection is unique. Taking the wrong antibiotic, or an incomplete dose, is ineffective and risky. Safely dispose of any leftovers at a pharmacy take-back program.

DON’T share your antibiotics with anyone else. It’s illegal and dangerous. The antibiotic was prescribed for your specific infection, at your specific dose, for your body. Sharing can cause allergic reactions, inappropriate treatment, and contribute to resistance.
DON’T assume a different antibiotic is interchangeable. If you had an antibiotic that worked for a past infection, it doesn’t mean it’s right for a new one. The bacteria might be different. Trust your doctor’s current prescription.
The Big Picture: You Are a Guardian of Public Health

Every time you use an antibiotic correctly, you’re not just healing yourself—you’re protecting the community. You’re helping to ensure these life-saving drugs remain effective for your children, your neighbors, and for future medical procedures like surgeries and cancer treatments that rely on antibiotics to prevent infections.
Your Action Plan:
1. Verify the infection is bacterial before starting.
2. Adhere religiously to the instructions.
3. Complete the full course, no matter what.
4. Dispose of leftovers safely.
5. Prevent infections in the first place through good hand hygiene and recommended vaccinations.
Antibiotics are a shared resource. Their power depends on our collective responsibility. By following these do’s and don’ts, you become a crucial part of the solution, safeguarding these medical marvels for generations to come.
FAQs
1. If I feel better after a few days, why is it dangerous to stop my antibiotics?
Feeling better means the medication is working and has killed the most vulnerable bacteria. However, the toughest bacteria may still be lingering. Stopping early allows these survivors to recover, multiply, and cause a relapse that is harder to treat. The full course is designed to ensure complete eradication.
2. Can antibiotic resistance affect me personally, or is it just a global problem?
It affects you directly. If you help create resistant bacteria by misusing antibiotics, those same bacteria can cause a second, much harder-to-treat infection in your own body. Furthermore, you could acquire a resistant infection from others in your community or in healthcare settings, limiting treatment options when you need them most.
3. How can I tell if my infection is viral or bacterial? I don’t want to bother my doctor.
You cannot reliably tell the difference yourself. This is exactly why you need a healthcare professional. Key signs a doctor looks for include: symptom duration (bacterial infections often follow or prolong viral ones), specific symptoms (like colored mucus or a certain type of sore throat), and sometimes tests (like a strep culture). It’s never a “bother” to get an accurate diagnosis.
4. What should I do if I miss a dose?
Take it as soon as you remember. However, if it’s almost time for your next dose, skip the missed dose and take the next one at the regular time. Do NOT double the dose. Doubling up can increase side effects without improving efficacy. Then, continue with the rest of your course as scheduled.

5. Is it really that bad to share antibiotics with a family member who has similar symptoms?
Yes, it’s dangerous and illegal. Symptoms can be similar for very different infections. The dose is calculated for the individual’s age, weight, and kidney function. Sharing can lead to: 1) Ineffective treatment, 2) Serious allergic reactions, 3) Unnecessary side effects, and 4) It directly contributes to antibiotic resistance. Never share prescription medications.
6. How should I safely dispose of leftover antibiotics?
The best option is a pharmacy take-back program. Many pharmacies have kiosks for safe medication disposal. If not available, the FDA recommends mixing the pills with an unappealing substance like used coffee grounds or cat litter in a sealed bag before throwing them in the trash. Do not flush them down the toilet unless the label specifically instructs you to do so, as this can contaminate water supplies.

7. Do probiotics help prevent antibiotic side effects like diarrhea?
The evidence is mixed but promising. Antibiotics can kill good gut bacteria along with the bad, leading to diarrhea. Some studies show certain probiotic strains (like Lactobacillus and Saccharomyces boulardii) can help maintain gut balance. It’s generally considered safe for most people, but always ask your doctor or pharmacist for a specific recommendation that won’t interfere with your medication.
8. Can I drink alcohol while on antibiotics?
It’s best to avoid alcohol completely during your course. While only a few antibiotics (like metronidazole) cause a severe reaction with alcohol, mixing can: 1) Increase side effects like nausea and dizziness, 2) Stress your liver, which is processing the medication, and 3) Potentially reduce the drug’s effectiveness. When in doubt, abstain until you finish.
9. What does “Take with Food” or “Take on an Empty Stomach” actually mean?

· With Food: Take the pill during a meal or with a snack. This helps buffer the stomach and prevent nausea.
· Empty Stomach: Take the pill 1 hour before eating or 2 hours after a meal. Food can interfere with the absorption of some antibiotics. If the label says this, it’s critical for effectiveness.
10. Are there really no new antibiotics being developed to replace the resistant ones?
The pipeline is dangerously thin. Developing new antibiotics is scientifically challenging, time-consuming, and not very profitable for drug companies compared to other medicines. This makes preserving our current antibiotics through responsible use even more urgent. Resistance will eventually outpace development if we are not careful.
11. What’s the single most important thing I can do to fight antibiotic resistance?
Use antibiotics only when absolutely necessary, and when prescribed, take them exactly as directed. Prevention is equally key: Wash your hands regularly and get recommended vaccines (like the flu shot and pneumococcal vaccine) to avoid infections in the first place.
12. My doctor said I don’t need an antibiotic. Does that mean they aren’t taking my illness seriously?
Absolutely not. It means your doctor is being a good steward of your health and public health. Prescribing an antibiotic for a viral infection offers zero benefit, exposes you to potential side effects, and puts you at risk for future resistant infections. A doctor who prescribes responsibly is providing the highest standard of care.