You’ve seen it at the pharmacy counter: your doctor prescribes a medication, and the pharmacist asks, “Would you like the generic version?” Often, it’s significantly cheaper. But a nagging question follows: Is it really as good?
Many of us hesitate, believing that a lower price must mean lower quality, or that the brand-name version is somehow “stronger” or “more reliable.” These misconceptions can cost us hundreds, even thousands, of dollars each year. Let’s clear the air and look at the facts.
The Core Truth: They Are Therapeutically Equivalent

Here’s the most important point: In the United States, generic drugs are required by the FDA to be bioequivalent to their brand-name counterparts. This means:
· Same Active Ingredient: The chemical that makes the drug work is identical in dosage, strength, and form (pill, liquid, injection).
· Same Safety & Efficacy: It must work the same way in the body and provide the same clinical benefit.
· Same Quality Standards: Generics must meet the same rigorous standards for identity, strength, purity, and stability. Manufacturing facilities are held to identical FDA inspections.
Think of it like this: You can buy a brand-name ibuprofen (like Advil) or a store-brand ibuprofen. The box looks different, but the medicine inside is the same molecule, working identically in your body.
Busting Common Myths About Generics
Myth 1: “Generics are made in substandard factories.”
Fact: Up to 40% of generic drugs are actually manufactured by the same companies that produce the brand-name versions. The FDA conducts over 3,000 inspections annually worldwide, ensuring all facilities—brand or generic—comply with strict Good Manufacturing Practices.
Myth 2: “The fillers and binders are different and can cause side effects.”
Fact: While inactive ingredients (fillers, dyes, binders) can differ, the FDA requires they be safe. For the vast majority of people, these cause no issue. If you have a severe allergy (e.g., to a specific dye or gluten), you can discuss it with your pharmacist, who can check the formulation for you.
Myth 3: “If generics are the same, why do they look different?”
Fact: Trademark law prevents generics from looking identical to the brand-name drug. The color, shape, or packaging may differ, but the medicine inside is held to the same standard.
Myth 4: “My doctor prefers the brand, so it must be better.”
Fact: Doctors may develop a habit of prescribing a familiar brand name. However, studies and medical associations consistently affirm the therapeutic equivalence of generics. You can always ask your doctor, “Is a generic available and appropriate for me?”
Where Does the Savings Come From?
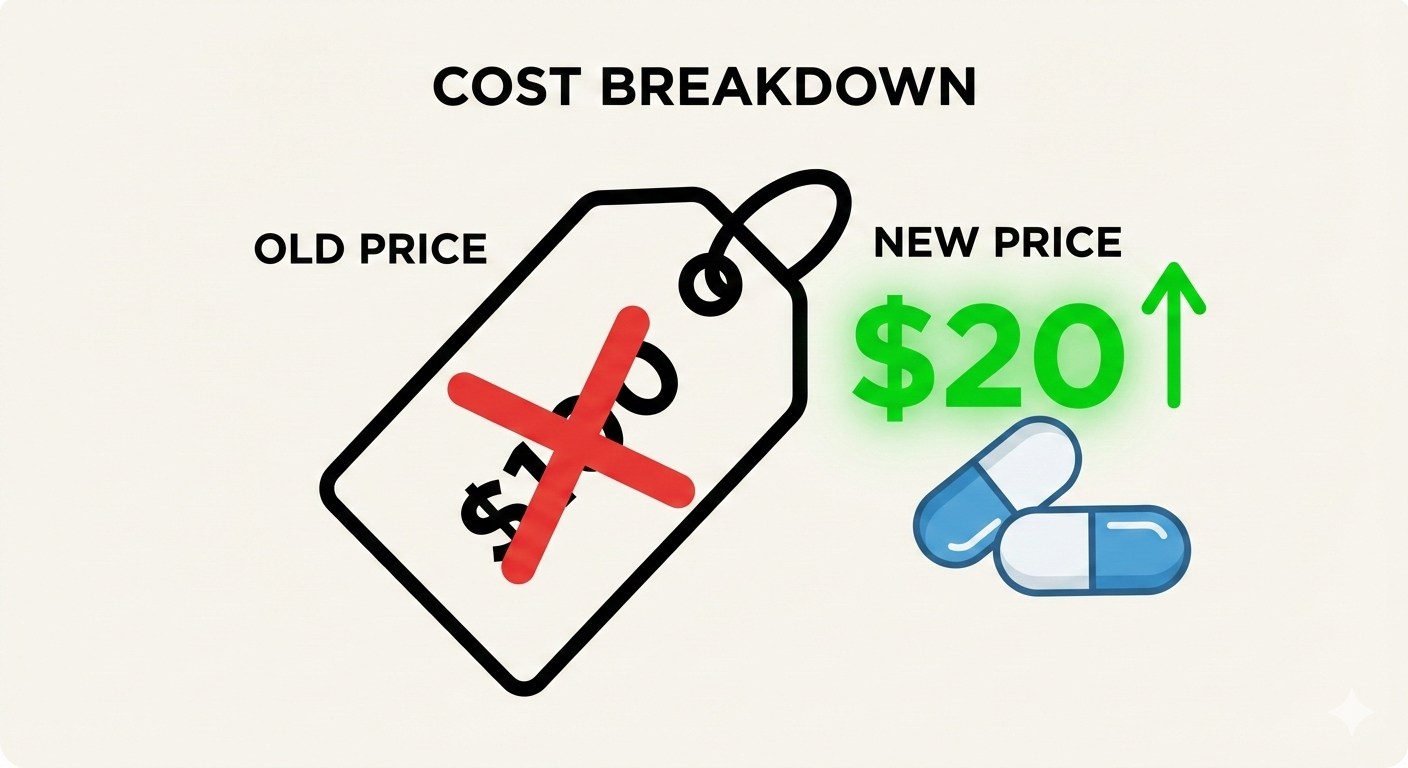
Developing a new brand-name drug is astronomically expensive, involving years of research, clinical trials, and marketing. This investment is protected by a patent. When the patent expires (usually after 10-15 years), other companies can apply to produce the generic. They don’t repeat the costly clinical trials, only proving bioequivalence. This competition drives prices down dramatically—often by 80-85%.
Those savings go directly into your pocket and help lower overall healthcare costs.
Are There Ever Exceptions?
In rare, specific cases, some healthcare providers may recommend a brand-name drug. This can involve:
· Narrow Therapeutic Index Drugs: For a few critical medications (like certain seizure or thyroid drugs), where tiny blood concentration differences matter, doctors may want to keep a patient on one consistent manufacturer (brand or generic).
· Patient Response: An individual might react differently to an inactive ingredient. This is uncommon but worth discussing with your doctor if you feel a noticeable change after switching.
The key is open communication with your healthcare team, not a blanket dismissal of generics.
The Bottom Line: Your Wallet & Your Health
Choosing an FDA-approved generic drug is a safe, effective, and financially smart decision. They are a cornerstone of modern healthcare, allowing millions greater access to essential medications.

At Your Next Pharmacy Visit:
1. Ask: “Is there a generic version of this prescription?”
2. Trust the rigorous science and regulation behind it.
3. Save your money for the things that matter most to you.
Your health doesn’t need a brand-name price tag. By understanding the facts, you can feel confident in the quality of generics and empowered to make choices that are good for both your body and your budget.
FAQs
1. Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove bioequivalence, meaning they work in the body at the same rate and to the same extent. The therapeutic effect is identical.

2. Why are generics so much cheaper?
Generics don’t repeat the expensive clinical trials and marketing campaigns that brand-name drugs do. Once a brand-name drug’s patent expires, generic manufacturers only need to prove bioequivalence. Increased competition drives prices down—often by 80-85%—while maintaining the same medical benefit.
3. If they’re the same, why do they look different (different color/shape)?
Trademark laws prevent generics from looking identical to the brand-name drug. The color, shape, or flavoring may differ due to different inactive ingredients, but the active pharmaceutical ingredient is the same. The appearance does not affect how the drug works.
4. Are the ingredients exactly the same?
The active ingredient is identical. Inactive ingredients (fillers, binders, dyes) may differ but must be approved by the FDA as safe. For most people, this causes no issue. If you have specific allergies (e.g., to dyes, lactose, gluten), ask your pharmacist to check the inactive ingredients.
5. Can switching to a generic cause side effects?
It’s uncommon. Since the active ingredient is the same, your body should react similarly. Rarely, someone might be sensitive to a change in an inactive ingredient. If you notice new or worsening symptoms after switching, contact your doctor. Often, perceived differences are due to the natural course of illness or the “nocebo” effect (expecting a negative outcome).
6. Do doctors and pharmacists trust generics?
Overwhelmingly, yes. Surveys show that healthcare professionals widely recommend generics. In the U.S., 9 out of 10 prescriptions are filled with generics—including those prescribed to doctors and their own families. Medical associations (like the AMA) endorse their use.
7. Are generic drugs made in lower-quality factories?
No. The FDA holds all drug manufacturing facilities—brand and generic—to the same strict Good Manufacturing Practice (GMP) standards. Many generics are made in the same factories as brand-name drugs. The FDA conducts regular inspections worldwide to ensure compliance.

8. Why did my pharmacist automatically switch me to a generic?
In most states, pharmacy laws or insurance contracts require or encourage automatic substitution with an FDA-approved generic unless the doctor specifically writes “Dispense as Written” or “Brand Medically Necessary” on the prescription. This is a standard cost-saving practice.
9. Are there any drugs where the brand matters?
In a small number of cases, doctors may prefer a patient stays on a specific manufacturer. This sometimes applies to narrow therapeutic index drugs (e.g., certain epilepsy, thyroid, or blood-thinning medications), where extremely precise dosing is critical. However, the FDA still approves generics for these drugs as bioequivalent. Any concern should be discussed with your doctor.
10. How can I be sure the generic I’m getting is safe, especially if it’s made abroad?
The FDA regulates all drugs sold in the U.S., regardless of where they are made. Foreign manufacturing sites are subject to the same FDA inspections as domestic ones. You can check the FDA’s Orange Book online to see all approved generic equivalents for a brand-name drug.
11. If I start on a brand-name drug, can I switch to a generic later?
In most cases, yes—and it’s a common way to save money. The switch is considered therapeutically equivalent. If you’re concerned, talk to your doctor or pharmacist. They can often provide guidance and reassurance.
12. Do insurance companies require generics?
Most insurance plans have generic-first policies (tiered formularies) where generics have the lowest copay. They may charge a significantly higher copay for a brand-name drug when a generic is available. Using the generic aligns with your insurer’s goal of controlling costs while providing effective care.
Bottom Line: FDA-approved generic drugs are a safe, effective, and smart financial choice. They undergo a rigorous approval process to ensure they perform identically to their brand-name counterparts. When in doubt, have an open conversation with your doctor or pharmacist—they are your best resource for personalized advice.

